-
PDF
- Split View
-
Views
-
Cite
Cite
Ameer Awashra, Zaid Sawaftah, Ali Bani Odah, Ahmed Sawafta, Amer Khatib, Huthayfa Dababat, Anas Yasin, Jehad Khamaysa, Muath Daraghmeh, Spontaneous splenic rupture as a primary manifestation of angiosarcoma: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae633, https://doi.org/10.1093/jscr/rjae633
Close - Share Icon Share
Abstract
Angiosarcoma, a rare endothelial cell tumor, accounts for < 2% of all sarcomas, typically affecting elderly patients. We present the case of a 62-year-old male with a history of hypertension and ischemic heart disease, who initially presented with severe lower back pain. Subsequent imaging revealed a ruptured splenic lesion and multiple liver lesions, leading to a diagnosis of stage 4 angiosarcoma. Post-splenectomy, the patient exhibited pathological vertebral fractures and elevated liver function tests, consistent with metastatic disease. Despite aggressive surgical intervention and supportive care, the patient’s condition remained critical. The treatment plan included palliative chemotherapy, spine radiotherapy, and ongoing pain management, with close monitoring of disease progression and response to therapy. This case describes the diagnostic challenges and poor prognosis associated with metastatic angiosarcoma.
Introduction
Angiosarcoma, also known as malignant hemangioendothelioma or visceral vascular tumor, is a rare endothelial cell tumor. It accounts for < 2% of all endothelial tissue sarcomas. The tumor is further classified based on its location: visceral (in muscles or skin) or non-visceral (in the liver, spleen, and other organs). Typically diagnosed in the elderly, angiosarcoma often presents as head and neck cancer. Although it rarely originates in the gastrointestinal tract, its diverse clinical manifestations can make diagnosis challenging. Symptoms may include abdominal pain, nausea, and recurrent gastrointestinal bleeding. Notably, no documented cases have been reported in Palestine [1–6].
In this context, we present a specific case study for a 62-year-old male with a complicated past medical history, presented with severe lower back pain, managed conservatively. He later developed severe colicky pain, and imaging revealed a ruptured splenic lesion and metastatic liver lesions. An urgent splenectomy confirmed stage 4 angiosarcoma. Postoperatively, the patient had pathological vertebral fractures and elevated liver function tests, leading to a treatment plan of palliative chemotherapy, spine radiotherapy, and ongoing pain management.
Case presentation
A 62-year-old male patient with a known history of hypertension and ischemic heart disease, status post coronary artery bypass grafting 3 years prior, initially presented with severe lower back pain. Upon evaluation in the emergency room, the patient reported a significant history of chronic back pain over the past three months, which had previously been investigated with MRI and CT scans, revealing lumbar disk issues. This back pain was treated conservatively with pain management and physical therapy. He had also been managed with conservative treatment for hypertension and ischemic heart disease, including medications and lifestyle modifications.
A few weeks later, the patient presented with severe, intermittent colicky pain in the left upper quadrant. MRI and CT scans indicated a ruptured splenic lesion accompanied by a subcapsular hematoma (see Fig. 1). Given the critical nature of his condition, an urgent exploratory laparotomy was performed. The surgery revealed approximately one liter of blood in the abdominal cavity due to venous bleeding from the ruptured splenic lesion. A splenectomy was performed, and multiple large liver lesions suggestive of metastatic disease were noted (see Fig. 1).
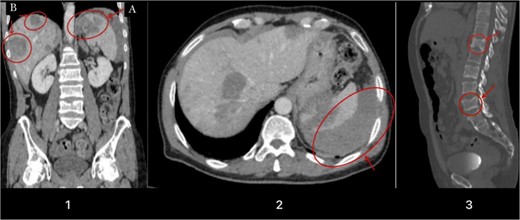
Illustrates a contrast-enhanced image obtained during the portal venous phase CT scan. Noteworthy findings include a hypodense lesion in the upper pole of the spleen (Image 1A), multiple liver lesions (Image 1B), evidence of a capsular laceration with adjacent free fluid indicative of intraperitoneal hemorrhage (Image 2), and compression fractures noticed on the vertebral body of T12 and L4 due to metastasis (Image 3).
The resected specimens, including the spleen, liver, and mesenteric biopsy, were submitted for histopathological examination. The findings revealed a diagnosis of stage 4 angiosarcoma. This malignancy is characterized by dense and hypercellular proliferation of spindle-shaped and epithelioid cells, with numerous mitotic figures. Immunohistochemical staining demonstrated positivity for vascular markers CD34 and CD31.
Postoperatively, the patient was transferred to the intensive care unit in critical condition. His status was complicated by severe back and hip pain that warranted further imaging and laboratory tests. These tests confirmed pathological vertebral fractures at T12 and L4 (see Fig. 1) and elevated liver function tests, supporting the diagnosis of metastatic disease. Despite aggressive surgical intervention and supportive care, the patient’s condition remained critical.
The treatment plan included an urgent referral to oncology for palliative chemotherapy and spine radiotherapy. The patient was maintained on a pain management regimen, including Tramadol and morphine. Follow-up plans included regular monitoring of liver function tests and imaging to assess the progression of metastatic disease. The patient’s response to palliative chemotherapy and radiotherapy was to be closely monitored, with adjustments to the treatment plan as needed.
Discussion
Angiosarcoma are mesenchymal tumors formed in blood vessel endothelial cells. There are two forms of angiosarcoma: visceral and non-visceral. Visceral angiosarcoma can affect the spleen, liver, heart, lungs, and bones; non-visceral angiosarcoma can affect the skin, subcutaneous tissues, and muscle tissues [7]. A very uncommon mesenchymal malignant tumor of vascular endothelial origin is splenic angiosarcoma. It may manifest as a secondary tumor coming from the skin, soft tissues, or bone, or as a primary tumor of the spleen. It is the most common non-lymphoid tumor of the spleen, regardless of its rarity. There is no hereditary predisposition and a small male preponderance with a mean age of presentation ranging from 50 to 79 years [2].
The majority of angiosarcomas develop spontaneously without any known risk factors, yet there have been situations where they develop from benign hemangiomas or chronic hematomas. Radiation-associated sarcoma usually develops 5 to 10 years after radiation exposure, but recent reports have suggested that a shorter time interval may also be possible, particularly with a history of concurrent chemotherapy [8]. However, there is no evidence that these factors were involved in this patient.
The clinical presentation is nonspecific and can range from splenic rupture and fatal bleeding to asymptomatic issues found after tests for unrelated reasons. A group of patients had almost 75% of them present with left upper abdomen pain and back pain, making it one of the most prevalent presenting symptoms. Anorexia, weakness, and weight loss are further potential concerns. Physical examination revealed splenomegaly as the most frequent symptom, as present in our case, along with hepatomegaly, and a palpable left upper quadrant mass can often be revealed [9]. The most common lab abnormalities are anemia and thrombocytopenia [10, 11], as in our case.
The poorest prognosis is related to traumatic rupture of the spleen in angiosarcoma patients, as there is an immediate risk of death from hypovolemic shock and disseminated intravascular coagulopathy. Moreover, it raises the possibility of hemorrhagic and peritoneal spreading. The range of reported metastatic rates is 69% to 100%. The bone marrow, liver, and bone are among the common metastatic locations [11, 12]. In our case, the patient underwent splenectomy for traumatic rupture, and intraoperative findings showed multiple large liver lesions (metastasis).
Splenic angiosarcoma remains difficult to diagnose definitively before surgery. Biopsy is dangerous due to the possibility of bleeding and malignant seeding. Histological diagnosis is usually possible after a splenectomy, which is both diagnostic and therapeutic. Preoperative CT imaging is extremely useful for both diagnosis and acute assessment of problems. Splenic enlargement in the context of a heterogeneous mass is common, with 60% of patients demonstrating this. Contrast CT scanning may indicate non-enhancing areas due to necrosis or enhancement with a blush, indicating ongoing bleeding. Metastases can also be identified on imaging, and they are present at the time of diagnosis in most cases. Similar radiological abnormalities can be found in lymphomas and metastatic disease with splenic involvement [2].
The best option of treatment for localized disease is splenectomy. A common diagnosis of metastasis indicates a poor prognosis. Despite treatment, the 5-month median survival rate is still quite low. However, metastatic angiosarcoma, as in our case, are difficult to manage and outcomes remain poor overall, for certain cases, with multi-modality treatment consisting of surgery, radiation, and chemotherapy, meaningful disease control and survival can be achieved [4].
Conclusion
We are describing the aggressive nature and diagnostic challenges of angiosarcoma, a rare and highly malignant endothelial cell tumor. The patient’s presentation with severe lower back pain, followed by a ruptured splenic lesion and multiple liver metastases, highlights the often insidious and varied manifestations of the disease. Despite prompt surgical intervention and aggressive palliative care, the prognosis remains poor due to the advanced stage at diagnosis and high metastatic potential of angiosarcoma. This case emphasizes the need for heightened clinical awareness and consideration of angiosarcoma in differential diagnoses of unexplained back pain and splenic lesions, especially in patients with a complex medical history.
Acknowledgements
We express our deep gratitude to the medical ward staff for their invaluable support in completing this report.
Conflict of interest statement
The authors state that they have no conflict of interest to be mentioned.
Funding
No specific grant from funding agencies was received for this work.
Ethics approval
Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent
Written informed consent was obtained from the patient Himself for his anonymized information to be published in this article.



