-
PDF
- Split View
-
Views
-
Cite
Cite
Nadia El-Diaz, Meera Goutham, Hemant Sheth, Importance of high suspicion of intestinal perforation in blunt abdominal injury in patients with inflammatory bowel disease, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae630, https://doi.org/10.1093/jscr/rjae630
Close - Share Icon Share
Abstract
Estimated to affect 3 million individuals in Europe alone, Crohn’s disease is an inflammatory bowel disease causing transmural inflammation throughout the gastrointestinal tract. We describe the case of a patient with a known background of Crohn’s disease who presented with abdominal pain following blunt abdominal trauma after a hit and run where initial diagnosis of perforation was missed on pan-computed tomography, however, diagnosis was made early due to high clinical suspicion of perforation. This suggests that current diagnostic imaging can be inaccurate, leading to delays where urgent surgery is otherwise indicated which is a cause for concern. Herein, we emphasize the importance of a high index of suspicion for perforation in patients with blunt abdominal trauma, especially where there is underlying bowel disease.
Introduction
Crohn’s disease is a chronic inflammatory condition which can cause inflammation throughout the gastrointestinal tract. It is estimated to affect at least 2.5 to 3 million individuals in Europe alone with rising incidence in younger populations [1, 2]. Intestinal perforation albeit rare (1%–3%) is a known risk in inflammatory bowel disease, commonly as a result of chronic inflammation, stenosis, and ulceration [2, 3]. Optimal medical and surgical therapy can significantly reduce the risk of perforation.
Case report
A 28 year old man with a four year history of Crohn’s disease on azathioprine and infliximab self-presented to our London general district hospital with abdominal pain after he was hit by a car whilst walking. On admission, he was drowsy and tachycardic but haemodynamically stable. Examination revealed guarding and rebound tenderness in the right iliac fossa.
Initial pan-computed tomography (CT) reported ‘no acute injury in the head, neck, chest, abdomen and pelvis’. Due to concern of perforation from examination, we requested a second review of the CT. The addended CT reported ‘bowel wall thickening in the terminal 20 cm length of ileum in keeping with known Crohn’s disease in this region but there appears to be an acute complication of possible evolving perforation of a focal area of distal ileum ~17 cm proximal to the ileocecal junction. There is an out-pouching of the gas in this region through the transmural inflammation and there is mild surrounding mesenteric inflammation’ (Fig. 1).
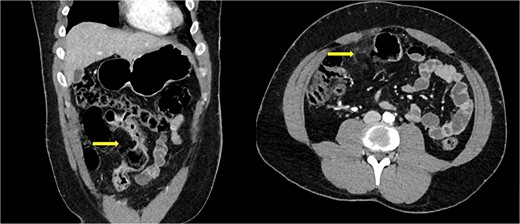
Abdominal computed tomography of coronal and axial cuts showing bowel perforation (arrow).
The case was discussed with a colleague general surgery consultant in our local tertiary centre who advised to watch-and-wait due to the evolving nature of the perforation but to reconsider surgery if the patient deteriorates.
Nine hours after the initial surgical review, the patient became febrile and tachycardic. Inflammatory markers had worsened despite broad-spectrum antibiotics. As a result, he was prepared for an emergency laparotomy. Intraoperatively, we found a small ileal perforation at the mesenteric border, ~30 cm from the ileocaecal junction with overlying attached omentum, sealing off the perforation (Fig. 2). There was no evidence of generalized peritonitis or peritoneal contamination. The rest of the terminal ileum was consistent with Crohn’s disease up to the ileocecal junction.

Photographic imaging showing the site of perforation in the small bowel.
He underwent a right hemicolectomy and side-to-side anastomosis of the ileum to transverse colon (Fig. 3). Manual palpation confirmed there was no Crohn’s disease at the site of anastomosis, later confirmed by histology. Initial decision to defunction was made given Crohn’s disease and ongoing immunotherapy. However, there was difficulty bringing the stoma out as when the small bowel loop was delivered along the ascending colon there was sudden mottling of the small bowel and ascending colon with weak mesenteric pulse, which recovered with warm packing. This was due to thickened and shortened mesentery from Crohn’s. Therefore, a decision for primary anastomosis of the ileum and transverse colon was made.

The patient spent one day in the intensive care unit. He was discharged eight days after surgery. He was followed up six months later with no complications.
Discussion
This case demonstrates a low sensitivity of CT for perforation in patients with underlying bowel inflammation, especially in the first few hours after trauma highlighting the importance for a high index of suspicion of perforation in patients with Crohn’s in the context of blunt abdominal trauma. This suspicion should also be extended to other conditions of chronic inflammation such as ulcerative colitis and diverticulitis in older populations.
To the best of our knowledge, this is the first missed CT intestinal perforation in a symptomatic patient with blunt abdominal trauma. A previous case report by Foula et al. [4] demonstrates a missed perforation on CT in a non-peritonitic patient with underlying Crohn’s after traumatic abdominal injury. Given the increased incidence of Crohn’s globally, it is important that bowel perforation is not missed to ensure early and optimal management and reduced hospital stay [5].
Studies have shown 80% sensitivity of CT in diagnosing bowel perforation [6, 7]. Delays in urgent surgery, where bowel perforation has been missed, has been linked to mortality [8, 9]. This is especially important in Crohn’s if imaging is completed soon after trauma [10]. There are many studies outlining the key CT findings in non-traumatic bowel perforation but there is a need for guidance on the CT findings to consider in blunt abdominal trauma in inflammatory bowel disease to prevent delays in urgent surgery [6]. Fortunately, in this case the symptoms were highly indicative of perforation and so a second opinion on the CT imaging was sought early leading to rapid surgical management.
Delayed urgent surgery in patients on immunotherapy and underlying bowel disease can lead to poor outcomes further emphasizing the importance of early diagnosis. The advent of corticosteroid therapy in the management of Crohn’s has significantly improved morbidity, especially in acute inflammation, but can increase the risk of post-operative infection and healing especially in urgent surgery if not stopped for more than 30 days prior to surgery [11]. A study by Selvasekar et al. [12] has demonstrated increased risk of post-operative infection in patients taking infliximab arising by multivariate analysis. In contrast, a study by Columbel et al .[13] has suggested that infliximab does not contribute to post-operative risks. Peri and post-surgical care of immunosuppressed patients with Crohn’s undergoing urgent surgery for traumatic perforation has not been clearly delineated but is important to define.
The value of imaging in acute abdominal pain is invaluable both in and out-of-hours in guiding surgical management. But no single optimal diagnostic test for perforation in blunt abdominal injury in patients with underlying inflammatory abdominal disease has been characterized. Abdominal pain, peritonitis, raised inflammatory markers, sepsis and haemodynamic instability should raise suspicion but may take several hours to manifest. We recommend intentional feedback loops amongst the multidisciplinary team to support monitoring and diagnosing perforation and therefore timely surgical management. Thorough review of imaging is vital, especially if clinical presentation does not correlate with a high index of suspicion for perforation in these patients. Evidence-based guidance of the CT findings to suggest perforation in this patient group is important for rapid diagnosis and optimal prognosis.
Conflict of interest statement
None declared.
Funding
None declared.



