-
PDF
- Split View
-
Views
-
Cite
Cite
Yavor Asenov, Ivan Vasilev, Theophyl Sedloev, Nikolay Penkov, Boris Kunev, Effective percutaneous treatment of severe necrotizing pancreatitis: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae627, https://doi.org/10.1093/jscr/rjae627
Close - Share Icon Share
Abstract
Necrotizing pancreatitis (NP) is a severe form of acute pancreatitis associated with high morbidity and mortality. The management of infected necrotizing pancreatitis (INP) has evolved from open surgical necrectomy to minimally invasive techniques, such as percutaneous catheter drainage (PCD). We report the case of a 71-year-old male with a history of cholelithiasis who presented with acute abdominal pain, nausea, and vomiting. Initial imaging revealed an enlarged pancreas with peripancreatic fluid collections. Conservative treatment improved his condition, but nine days later signs of sepsis, including a persistent fever were presented. Computed tomography (CT) verified several large gas-containing fluid collections spreading from the pancreas to the left iliac crest along with bilateral pleural effusions. The patient underwent PCD with multiple drains inserted. Microbiological analysis showed Meropenem-resistant E. coli, leading to a change in antibiotic therapy. Follow-up imaging confirmed the resolution of fluid collections, and the patient recovered without requiring laparotomy. PCD has emerged as a crucial component of the step-up approach in managing INP. Compared with open necrectomy, PCD offers lower mortality and morbidity rates. The PAncreatitis, Necrosectomy versus sTEp up appRoach (PANTER) trial and subsequent studies have validated the efficacy of PCD, demonstrating its ability to reduce complications and healthcare costs while improving patient outcomes. PCD is a safe and effective treatment for INP, representing a valuable alternative to traditional surgical methods. This case underscores the importance of minimally invasive strategies in the management of NP.
Introduction
Necrotizing pancreatitis (NP) is a severe and rapidly progressive form of acute pancreatitis characterized by the necrosis of pancreatic and peripancreatic tissue. This condition is associated with significant morbidity, mortality, and a high incidence of life-threatening complications. One of the most critical risk factors contributing to mortality in NP is the infection of pancreatic necrosis. Historically, the primary treatment for patients with infected necrotizing pancreatitis (INP) was surgical necrectomy via laparotomy, aimed at removing all infected necrotic tissue. However, this approach was associated with high morbidity and mortality rates reaching 40% [1].
With advancements in minimally invasive techniques, the treatment paradigm for INP has shifted from open surgery to less invasive approaches. This step-up approach begins with conservative management and escalates to minimally invasive procedures as needed. The percutaneous catheter drainage (PCD), as part of this strategy, has shown promise in managing INP by effectively draining infected collections and reducing the need for extensive surgical intervention [1–10].
In this report, we present a case of acute INP treated with PCD, highlighting its safety, efficacy, and role within the step-up approach for managing necrotizing pancreatitis.
Presentation of case
We report a case of a 71-year-old male patient with a history of cholelithiasis, who presented to the emergency department with acute abdominal pain located in the epigastric region and right hypochondrium, radiating to the back, accompanied by nausea and repeated vomiting. Physical examination revealed tenderness to palpation in the upper abdomen without signs of peritoneal irritation. Laboratory findings showed leukocytosis (19.18 G/L) with neutrophilia (17.32 G/L), high levels of serum amylase (2622 U/L), hyperglycemia (8.31 mmol/L), mild hyperbilirubinemia (total – 37 μmol/L, direct – 20.7 μmol/L), and hypertransaminasemia (ASAT – 301 U/L, ALAT – 364 U/L). Abdominal ultrasound revealed an enlarged pancreas with a blurred hypoechoic echostructure, indistinct gland margin, peripancreatic fluid, and abdominal free fluid located in the subhepatic and subphrenic spaces and in the pelvis. Additional sonographic findings included known cholelithiasis with gallbladder sludge without signs of cholecystitis and a slightly dilated common bile duct (1 cm). Conservative treatment, including fluid replacement, nutritional support, and pain management, was initiated, resulting in an improvement of the clinical condition and blood tests.
Nine days later, a persistent fever reaching 38.6°C with tenderness in upper abdominal quadrants was presented. In addition, the patient reported significant fatigue and exhibited tachycardia with a heart rate of up to 106 beats per minute. Laboratory findings revealed leukocytosis (15.03 G/L) with neutrophilia (11.84 G/L), moderately elevated serum amylase (394 U/L), and hyperbilirubinemia (total – 31.7 μmol/L, direct – 23.1 μmol/L). Abdominal ultrasound showed an enlarged pancreas with blurred, heterogeneous hypoechoic echostructure, indistinct gland margin, peripancreatic fluid, and walled-off necrosis next to the pancreatic tail, extending laterally to the splenorenal recess, with a longitudinal size of ~10 cm and thick heterogeneous content, suggesting secondary inflammation. Computed tomography (CT) verified gas-containing fluid collections spreading from the pancreas to the left iliac crest (Fig. 1A and B) along with bilateral pleural effusions.
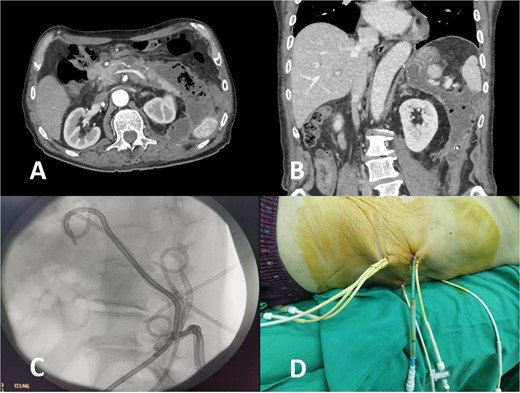
CT image of large infected peripancreatic collections with multiple air locules (A and B) and placed pigtail catheters post-imaging (C and D).
Following well-established guidelines, empiric antibiotic therapy with a carbapenem was started (Meropenem 1 g every 8 hours). The patient underwent PCD with the initial insertion of five drains: two in the peripancreatic collection and three in the pararenal space, with one situated caudal to the lower border of the collection at the level of the iliac crest. Microbiological examination revealed the presence of Meropenem-resistant Escherichia coli, sensitive to Cefoperazone-sulbactam, necessitating a change in antibiotic treatment according to antibiogram results. Continuous postprocedural transcatheter lavage with physiological saline was performed. Follow-up abdominal sonography showed the persistence of a small undrained collection in the posterior pararenal space, leading to the placement of two additional drains in that area (Fig. 1C and D).
A subsequent microbiological examination showed no bacterial growth. Normal laboratory findings. Additional abdominal ultrasound and CT showed no significant remaining fluid collections (Fig. 2).
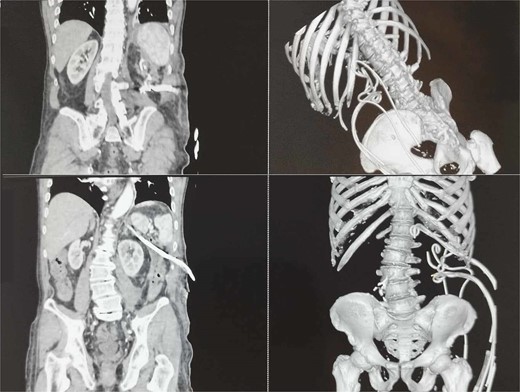
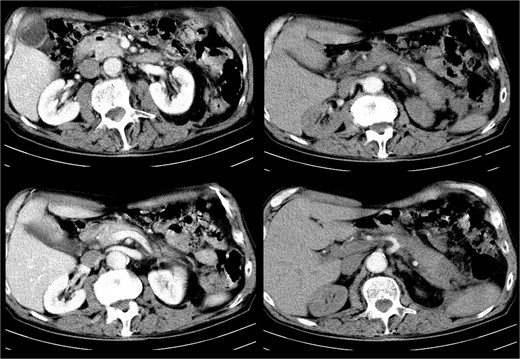
The patient recovered gradually, and no laparotomy was required. A follow-up CT after one month showed no residual collections (Fig. 3).
Discussion
PCD for NP was first described by Freeny et al. [2] in 1998 with a reported success rate of 47%. Since then, the step-up approach has gained acceptance [1]. Initial treatment of acute NP typically includes empiric antibiotic therapy, followed by minimally invasive strategies when infected necrosis is suspected. This approach was validated by the multicenter randomized clinical trial PANTER, which demonstrated that the step-up management of NP significantly reduces patient mortality, multi-organ failure, healthcare costs, and late surgical complications [3].
The PAncreatitis, Necrosectomy versus sTEp up appRoach (PANTER) trial highlighted the importance of early drainage, although it emphasized that indications for such procedures should be carefully confirmed to avoid converting sterile collections into infected ones. Following these guidelines, it has been observed that up to 35% of patients with INP can be treated with PCD alone, thus avoiding necrectomy and its associated complications [1].
Necrectomy by laparotomy, traditionally the standard treatment for INP, is associated with high mortality rates (15%–27%) and considerable morbidity [4]. In contrast, a retrospective multicenter study involving 11 hospitals in the Netherlands found that minimally invasive surgery, including continuous postoperative lavage (CPL), resulted in significantly lower mortality rates (11%) compared with laparotomy and CPL (25%) [5]. This supports the shift towards less invasive methods.
Further evidence of the efficacy of PCD comes from a study demonstrating a 15% mortality rate and a 70% success rate in patients undergoing this procedure for infected pancreatic necrosis [6]. According to a report by Baudin et al. [2], which included 48 patients who underwent CT-guided percutaneous drainage for INP, the success rate was 64.6%. These findings underscore the potential of PCD to effectively manage INP with lower risk and better outcomes compared with traditional surgical approaches.
The safety and efficacy of PCD are further supported by additional studies. For instance, a systematic review conducted by Ke et al. [8] confirmed the role of PCD in reducing the need for surgical intervention, highlighting its effectiveness in managing pancreatic necrosis and associated collections. Ai et al. [9] demonstrated the utility of ultrasound-guided PCD in the early treatment of severe acute pancreatitis, noting its impact on improving patient outcomes and reducing hospital stay durations. Furthermore, Ganaie et al. [10] reported the effectiveness of image-guided PCD in managing acute pancreatitis-associated pancreatic collections, further solidifying the role of minimally invasive techniques in this context.
However, PCD has limitations, such as incomplete drainage, the potential for persistent infection, and the risk of complications such as fistula formation. In cases where PCD fails to adequately resolve the infection or drain the necrotic collections, escalation to more invasive procedures, such as an endoscopic or surgical approach, may be necessary.
Conclusion
PCD offers a viable, less invasive alternative to surgical necrosectomy for patients with INP. It is associated with lower mortality and morbidity rates, reduced healthcare costs, and improved patient outcomes. The step-up approach, starting with conservative management and escalating to minimally invasive interventions as needed, aligns with current evidence and clinical practice guidelines, providing a structured framework for managing this complex condition.
Conflict of interest statement
None declared.
Funding
None declared
References
- pancreatitis, acute
- pancreatitis
- surgical procedures, minimally invasive
- acute abdomen
- computed tomography
- pleural effusion
- acute abdominal pain
- fever
- follow-up
- health care costs
- laparotomy
- pancreatitis, necrotizing, acute
- surgical procedures, operative
- diagnostic imaging
- drainage procedure
- morbidity
- mortality
- pancreas
- meropenem
- persistence
- percutaneous catheters
- iliac crest
- kanavel's four cardinal signs
- cholelithiasis
- conservative treatment
- patient-focused outcomes
- verification



