-
PDF
- Split View
-
Views
-
Cite
Cite
Sofia Boligo, Cláudia Santos, Cláudia Branco, Helena Contente, Laparoscopic excision of an incidental vascular tumor, Journal of Surgical Case Reports, Volume 2024, Issue 10, October 2024, rjae624, https://doi.org/10.1093/jscr/rjae624
Close - Share Icon Share
Abstract
Anastomosing hemangioma (AH) is an exceedingly rare benign vascular tumor, often mistaken for malignant neoplasms due to its histological features. First described in 2009, AH has been documented in various sites, including the kidney, liver, and adrenal gland. This report presents a 64-year-old man who, following a bicycle accident, underwent imaging that revealed a nodule suspicious for a paraganglioma in the right para-caval region. Despite the high radiotracer uptake on 68Ga-DOTANOC PET scan, which suggested paraganglioma, the patient remained asymptomatic and laboratory tests ruled out excessive catecholamine secretion. Surgical excision led to a diagnosis of AH, distinguished by its unique anastomosing vascular pattern and histological similarity to angiosarcoma. This case underlines the diagnostic challenges and potential for overtreatment of AH, highlighting the need for heightened awareness and careful histopathological and imaging evaluation to avoid misdiagnosis and ensure appropriate management.
Introduction
Hemangiomas are benign vascular tumors, most located in the skin and subcutaneous tissue. Visceral hemangiomas are uncommon and occur predominantly in the liver. Histologically, they have been classified as cavernous, capillary, or venous [1].
Anastomosing hemangioma (AH) is an extremely rare subtype of vascular tumor, histologically resembling angiosarcoma, first described in 2009, and initially attributed to the genitourinary system. Since its initial description, it has been identified in multiple other locations, including the adrenal gland, liver, colon, small intestine, and mesentery [2]. To date, ~120 cases have been reported in the literature, with ~60 occurring in the kidney [3].
The name derives from its unique histological characteristics, characterized by blood vessels resembling capillaries organized in a unique anastomosing pattern. The cells lining up the vessels are generally uniform, with minimal atypia and mitotic activity. These cells may also exhibit a “hobnail” morphology, associated with some malignant tumors, including renal cell carcinoma.
AH shows a slightly higher prevalence in women (1.38:1), with an average age of diagnosis of 53 years. Its average size is 2 cm and is generally unilateral, though it can occasionally appear bilaterally or multifocally [2]. These tumors are typically asymptomatic and found incidentally on imaging studies. Diagnosis is made through histopathological evaluation of a biopsy or surgical excision of the lesion.
Despite the increasing prevalence, this remains a poorly understood entity due to the absence of specific radiological and clinical manifestations, often leading to other differential diagnoses, and overtreatment.
Case report
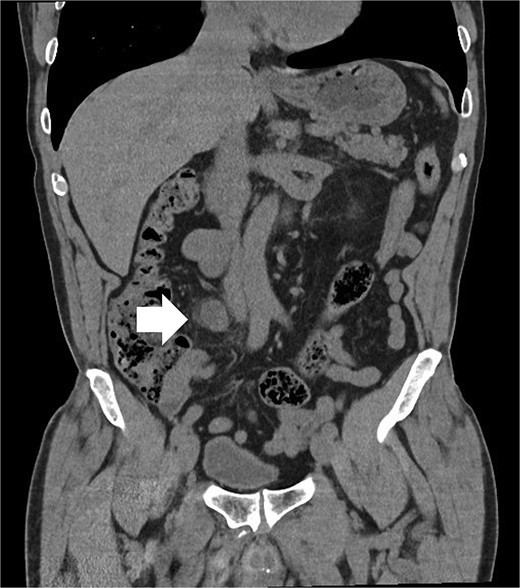
A 64-year-old man with a history of type 2 diabetes, dyslipidemia, and benign prostatic hyperplasia presented to the emergency department following a bicycle accident, resulting in left lumbar trauma. During the patient’s evaluation, an abdominal-perineal computed tomography (CT AP) was requested, which revealed: “Left perirenal hematoma without evidence of active extravasation. A 20x27x24mm nodule (T X AP X CC) in the right para-caval region, approximately at the level of the convergence of the common iliac veins, with heterogeneous and progressive enhancement, possibly indicating a paraganglioma/Zuckerkandl organ.” (Figs 1 and 2). The patient was admitted to the Urology department for conservative treatment, with good clinical evolution, and discharged after 5 days.

Following the incidental finding on the CT AP, and given the suspicion of paraganglioma, the patient was referred to Endocrinology, where blood and urine tests were requested (Table 1), along with a 68Ga-DOTANOC PET scan, which revealed: “Increased radiotracer uptake in a nodular density, approximately, 27 mm in the largest axial dimension, located in the para-caval region (SUV max 9.3), suggesting disease with increased somatostatin receptor expression.” The patient was asymptomatic, leading to a diagnosis of non-functioning paraganglioma and referral to General Surgery, where surgical excision of the lesion was proposed.
| . | Patient value . | Reference value . |
|---|---|---|
| Chromogranin A | <5 ng/mL | <100 ng/mL |
| Plasma metanephrine | ||
| Metanephrine | 23 pg/mL | <100 ng/mL |
| Normetanephrine | 77 pg/mL | <217 pg/mL |
| Plasma catecholamines | ||
| Epinephrine | 14 pg/mL | 20–60 pg/mL |
| Norepinephrine | 465 pg/mL | 300–650 pg/mL |
| Dopamine | 19 pg/mL | 10–150 pg/mL |
| Urine metanephrine | ||
| Metanephrine | 67 pg/24 h | <824 pg/24 h |
| Normetanephrine | 245 pg/24 h | <375 pg/24 h |
| Urine catecholamines | ||
| Epinephrine | 7 mcg/24 h | 18 mcg/24 h |
| Norepinephrine | 130 mcg/24 h | 76 mcg/24 h |
| Dopamine | 407 mcg/24 h | 390 mcg/24 h |
| . | Patient value . | Reference value . |
|---|---|---|
| Chromogranin A | <5 ng/mL | <100 ng/mL |
| Plasma metanephrine | ||
| Metanephrine | 23 pg/mL | <100 ng/mL |
| Normetanephrine | 77 pg/mL | <217 pg/mL |
| Plasma catecholamines | ||
| Epinephrine | 14 pg/mL | 20–60 pg/mL |
| Norepinephrine | 465 pg/mL | 300–650 pg/mL |
| Dopamine | 19 pg/mL | 10–150 pg/mL |
| Urine metanephrine | ||
| Metanephrine | 67 pg/24 h | <824 pg/24 h |
| Normetanephrine | 245 pg/24 h | <375 pg/24 h |
| Urine catecholamines | ||
| Epinephrine | 7 mcg/24 h | 18 mcg/24 h |
| Norepinephrine | 130 mcg/24 h | 76 mcg/24 h |
| Dopamine | 407 mcg/24 h | 390 mcg/24 h |
| . | Patient value . | Reference value . |
|---|---|---|
| Chromogranin A | <5 ng/mL | <100 ng/mL |
| Plasma metanephrine | ||
| Metanephrine | 23 pg/mL | <100 ng/mL |
| Normetanephrine | 77 pg/mL | <217 pg/mL |
| Plasma catecholamines | ||
| Epinephrine | 14 pg/mL | 20–60 pg/mL |
| Norepinephrine | 465 pg/mL | 300–650 pg/mL |
| Dopamine | 19 pg/mL | 10–150 pg/mL |
| Urine metanephrine | ||
| Metanephrine | 67 pg/24 h | <824 pg/24 h |
| Normetanephrine | 245 pg/24 h | <375 pg/24 h |
| Urine catecholamines | ||
| Epinephrine | 7 mcg/24 h | 18 mcg/24 h |
| Norepinephrine | 130 mcg/24 h | 76 mcg/24 h |
| Dopamine | 407 mcg/24 h | 390 mcg/24 h |
| . | Patient value . | Reference value . |
|---|---|---|
| Chromogranin A | <5 ng/mL | <100 ng/mL |
| Plasma metanephrine | ||
| Metanephrine | 23 pg/mL | <100 ng/mL |
| Normetanephrine | 77 pg/mL | <217 pg/mL |
| Plasma catecholamines | ||
| Epinephrine | 14 pg/mL | 20–60 pg/mL |
| Norepinephrine | 465 pg/mL | 300–650 pg/mL |
| Dopamine | 19 pg/mL | 10–150 pg/mL |
| Urine metanephrine | ||
| Metanephrine | 67 pg/24 h | <824 pg/24 h |
| Normetanephrine | 245 pg/24 h | <375 pg/24 h |
| Urine catecholamines | ||
| Epinephrine | 7 mcg/24 h | 18 mcg/24 h |
| Norepinephrine | 130 mcg/24 h | 76 mcg/24 h |
| Dopamine | 407 mcg/24 h | 390 mcg/24 h |
The patient underwent laparoscopic surgery, with intraoperative identification of a nodular formation above the right iliac artery and medial to the right ureter, measuring 3 cm, which was excised after opening the retroperitoneum and ligating the vascular pedicle. The postoperative course was uneventful, and the patient was discharged after 2 days.
Pathology revealed a benign vascular neoplasm, whose morphological pattern favored AH (Figs 3 and 4).
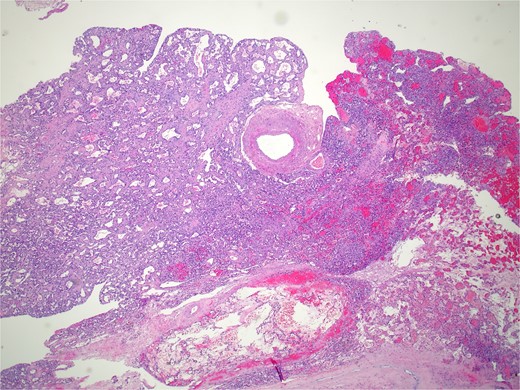
Histopathology micro findings showing anastomosing proliferation of capillary-sized vessels with mild endothelial cell nuclear variability.
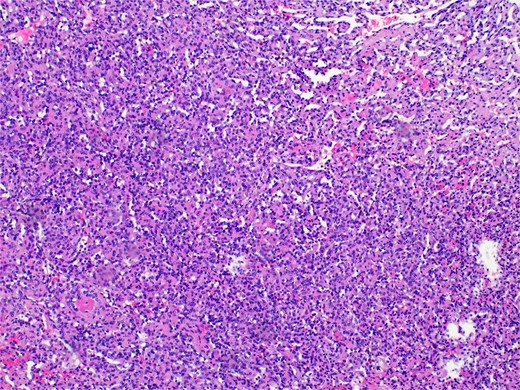
Histopathology micro findings showing scattered “hobnail” cells.
Discussion
The presented case describes an incidental finding during imaging evaluation. The initial computed tomography (CT) scan suggested a potentially significant lesion, leading to the suspicion of a paraganglioma, a rare neuroendocrine neoplasm that originates from neural crest cells and can secrete catecholamines, causing a range of clinical manifestations. However, the patient was asymptomatic, and subsequent laboratory tests showed no evidence of excessive hormonal production, supporting the diagnosis of a non-functioning paraganglioma.
The 68Ga-DOTANOC PET scan, which showed significant radiotracer uptake in the lesion, reinforced the initial suspicion of paraganglioma due to the high expression of somatostatin receptors, a common characteristic of this neoplasm. However, this finding is not specific to paragangliomas and can be observed in other vascular lesions, including AHs, although this is less common [4].
AH is a rare vascular neoplasm that can be easily mistaken for malignant tumors due to its histological and imaging characteristics. This case report illustrates the complexity of differential diagnosis in incidental vascular lesions, particularly when located in critical anatomical regions.
A multidisciplinary approach, involving specialists in radiology, endocrinology, surgery, and pathology, was essential in this case, from initial detection to definitive diagnosis. This report highlights the importance of meticulous histopathological evaluation and the careful use of imaging studies, such as 68Ga-DOTANOC PET, which, despite their high sensitivity, may lead to misinterpretations when not adequately contextualized.
The rare occurrence of AHs emphasizes the need for increased awareness of this entity among healthcare professionals, so it can be considered in future differential diagnoses. Further studies are necessary to elucidate the clinical behavior of this neoplasm and to develop management guidelines that can minimize unnecessary interventions and optimize patient outcomes.
Conflict of interest statement
The authors declare no conflicts of interest.
Funding
None declared.
References
- hemangiosarcoma
- positron-emission tomography
- hypertension
- hemangioma
- catecholamines
- adrenal glands
- cancer
- bodily secretions
- laboratory techniques and procedures
- laparoscopy
- paraganglioma
- neoplasms in vascular tissue
- diagnosis
- diagnostic imaging
- kidney
- liver
- benign neoplasms
- vascular tumor, benign
- bicycle accidents
- radiolabel
- misdiagnosis
- excision
- histopathology tests
- overtreatment



