-
PDF
- Split View
-
Views
-
Cite
Cite
Riccardo Bonomi, I Fabio Rapisarda, Areolar reconstruction: MICAP flap as a skin paddle donor site in skin sparing mastectomy and implant-based reconstruction, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad729, https://doi.org/10.1093/jscr/rjad729
Close - Share Icon Share
Abstract
The main advantage of preserving the nipple-areola complex (NAC) in small to moderate size breasts reconstruction is that the main diameters of the breast mound remain unaltered. When for oncological reason the NAC must be excised, a paddle of skin needs to be borrowed from a donor site and transferred into the surgical defect to maintain the breast contour. While this is easily achievable with the majority of autologous reconstructions, it is very challenging in the context of implant-based reconstructions, where the primary closure of the defect leads to a flattened breast mound and suboptimal cosmetic results. In our experience, the medial intercostal artery perforator flap enables the safe resection of the NAC with concurrent reconstruction of the defect, allowing a satisfactory cosmetic result in terms of contour and projection even in the setting of implant-based reconstruction.
Introduction
Nipple sparing mastectomy (NSMx) and immediate breast reconstruction has become the treatment of choice in eligible patients [1, 2].
Its safety is now well documented, and over the last decades, the adoption of this concept has widened, new techniques have been developed, indications have been expanded and a growing number of patients are currently offered this option [3, 4]. Two large surveys by Jagsi R et al. in 2015 and Atisha DM et al. in 2015 have now demonstrated a comparable degree of satisfaction between mastectomy and reconstruction and breast conserving surgery [5, 6].
Unfortunately, sparing the nipple-areolar complex (NAC) is not always oncologically safe and, therefore, it must be removed whenever the disease is in close proximity or infiltrating it. In these cases, a paddle of skin can be successfully used to replace the NAC and preserve the diameters and proportions of the reconstructed breast.
If the immediate reconstruction is performed through an autologous flap, part of the skin from the donor site can be used to replace the NAC, allowing the preservation of the contour of the breast. In the setting of implant-based immediate reconstruction, this is really challenging, and the loss of this disk of skin from the central part of the breast envelope can result in a significant reduction of the two main diameters of the breast mound and thus in a flattened contour of the reconstructed breast. While this is less relevant in patients with large and ptotic breasts, where skin reducing techniques can be used to tailor and reshape the excess of skin envelop in order to preserve the breast contour, this is not the case in small- to moderate-size breasts with minimal ptosis, where there is no excess of skin that can be successfully manipulated. To obviate this problem, we have devised a technique that allows us to transfer a paddle of skin on a pedicled flap from below the inframammary fold (IMF).
We are here describing the use of a round paddle of skin located on a medial intercostal artery perforator (MICAP) flap to replace the defect left by the removal of the NAC at the time of the mastectomy, which has allowed us to achieve significant cosmetic improvement in the reconstructed breast contour.
To our knowledge, this technique has not yet been described.
Case report
Clinical assessment
A 53-year-old woman underwent routine screening mammograms, which revealed three clusters of micro calcifications on the right breast. One was in the upper outer quadrant 7.5 cm from the nipple, one 3.5 cm from the nipple and the third one just behind the NAC. Ultrasound scan of the right breast was unremarkable. Stereo core biopsies confirmed intermediate to high degree DCIS in all three sites.
The MDT decision was to offer mastectomy plus or minus reconstruction and sentinel node biopsy, with removal of the NAC.
She was wearing a 34 C cup bra. The preoperatively sternal notch to nipple distance was 24 cm, and the nipple to mammary fold distance was 10 cm. The diameter of the areola was 6 cm.
Patient was explained that the removal of an NAC of such a diameter would have resulted in a flattened reconstructed breast. The patient was not suitable to have a DIEP flap and was not interested in exploring any other autologous reconstruction. Her preference was to have an implant-based reconstruction.
She was then consented to have the reconstruction of the areola using immediate MICAP flap reconstruction and was made aware that, if any complication occurred, the reconstruction would have been converted into a traditional one.
Preoperative marking
The neo-areola was marked immediately under the IMF of the right breast and medial to anterior axillary line. The MICAP flap was marked as per standard procedure and the medial intercostal arterial perforator was marked with Huntleigh Mini Dopplex D900.
The diameter of the skin disc used to form the neo-areola was marked using the standard 4-cm nipple marker (Fig. 1).
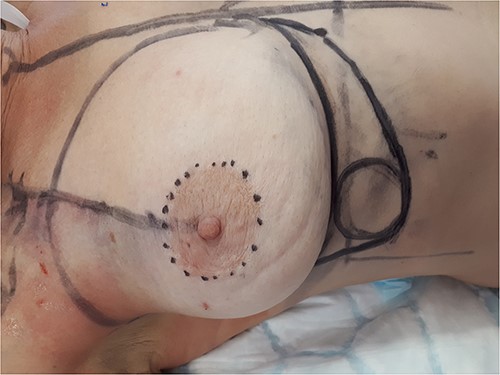
Preoperative marking. The new areola lays inferior to the IMF and medial to the anterior axillary line.
Surgical technique
Standard dual technique sentinel node biopsy using blue dye and radioisotope (Tc 99) was performed through a separate incision in the axilla retrieving two sentinel nodes and one palpable node.
Skin sparing mastectomy (SSMx) was performed through the infra-mammary fold and through the peri-areolar incision. The weight of the breast was 418gr (Fig. 2).

The SSMx is performed through the periareloar and IMF incisions.
The MICAP flap was de-epithelialized preserving the 4-cm paddle of skin to reconstruct the neo-areola. Then the MICAP flap was dissected until the neo-areola was easily transposable to replace the original NAC (Fig. 3). An abdominal advancement flap was performed to close the defect and recreate an IMF symmetrical with the contralateral one (Fig. 4).

The MICAP flap bearing the preserved disk of skin (new areola) is mobilized until it reaches the desired position.

The abdominal flap is mobilized and re-sutured to recreate the new IMF.
The breast volume has been replaced using a 500-cc Mentor® Becker 25 implant expander. This was initially inflated with only 100 ml of saline in order to avoid any internal compression of the flap (Fig. 5).

Pre-pectoral expander remains under-inflated to avoid the compression the the vascular pedicle of the MICAP flap.
One 10 French redivac drain was positioned on the chest wall at the level of the abdominal advancement flap and another one was left in the breast cavity.
Post-operative management and results
The drain in the abdominal advancement flap was removed at day 4 post surgery and the drain in the breast at day 8 post surgery. The expander implant was gradually inflated with saline within 3 weeks achieving a good symmetry with the contralateral breast (Fig. 6).

Early post-op results. The expander is fully inflated within 4–6 weeks, once the new areola is fully established.
There were no postoperative complications at 3 months, including any flap failure or necrosis, wound complications, seroma collection or infection.
The overall cosmetic results were extremely satisfactory for the patient and surgeons alike.
Discussion
SSMx with primary closure of the central defect after removal of the NAC results in a flattened reconstructed breast due to the excision of a significant amount of skin envelope in the most projected part of the breast.
NSMx offers superior cosmetic results when compared with a standard SSMx, as confirmed by the outcomes of the patients’ post-mastectomy QoL questionnaire [7]. The meta-analyses by Clarijs et al. showed significant differences in the Psychosocial Well-being and Sexual Well-being domains of the BREAST-Q in favor of NSMx [8].
When the NAC needs to be sacrificed, its replacement can be achieved even in immediate reconstruction with implants, using a paddle of skin from a pedicled flap; the MICAP flap is an ideal donor site in these cases, recreating a contour and a projection of the reconstructed breast which is matching the contralateral side.
Conflict of interest statement
None declared.
Funding
None declared.



