-
PDF
- Split View
-
Views
-
Cite
Cite
Wei Dai, Na Mei, Ye Ning, Wentian Zhang, Yan Li, Lei Jiang, Identifying the intersegmental plane for segmentectomy using the open insufflation technique, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad620, https://doi.org/10.1093/jscr/rjad620
Close - Share Icon Share
Abstract
Accurate identification of the intersegmental plane is the key to successful segmentectomy. This case series included 41 patients who underwent uniportal thoracoscopic segmentectomy using the open insufflation method to identify the intersegmental plane for pulmonary nodules. The median age of the patients was 58 (range 35–73) years, and 63.4% were female. Malignant pulmonary nodules accounted for 80.5% of cases and were staged as 0–IA2. Seventeen patients underwent a single subsegmentectomy or single segmentectomy, and 24 underwent combined subsegmentectomy or subsegmentectomy combined with segmentectomy. There was no conversion to multiportal video-assisted thoracoscopic surgery, open surgery, or lobectomy. The median operative time was 84 (range 45–194) min, and the median blood loss was 50 (range 10–150) ml. The median chest tube duration and postoperative hospital stay were 2 (range 1 − 7) days. One (2.4%) developed an air leak for >5 days. No deaths occurred within 30 days after surgery.
Introduction
Lobectomy is the standard procedure for early-stage lung cancer [1]. With the publication of the results of two large-scale randomized controlled trials [2, 3], segmentectomy as a lung parenchymal-sparing resection to lobectomy is becoming an alternative for small-sized (tumor diameter ≤ 2 cm) peripheral non-small-cell lung cancer. Segmentectomy is also a preferred procedure for centrally located small pulmonary tumors. However, anatomical segmentectomy is technically challenging because it involves complex segmental anatomy and accurate identification of the intersegmental plane (ISP) [4, 5].
There are six main methods to identify the ISP, each with merits and demerits [6]. The three most widely used methods are the modified inflation–deflation, indocyanine green fluorescence, and selective segmental inflation methods. However, the modified inflation–deflation method requires a relatively long waiting time and is not suitable for patients with emphysema; the indocyanine green fluorescence and selective segmental inflation methods require additional equipment and medical personnel [7]. Our team introduced a new method, called open insufflation, to identify the ISP, which may be simple and not time-consuming [8]. This study aimed to further investigate the feasibility and safety of this method in identifying the ISP for segmentectomy based on retrospective cohort data.
Case series
Patients who underwent segmentectomy using the open insufflation method to identify the ISP at our institution between December 2017 and May 2021 were retrospectively reviewed. Patients aged <18 years or with a history of chest surgery were excluded. Demographic characteristics, clinical variables, and perioperative outcomes were also assessed. The pathological stage of lung cancer was determined according to the eighth edition of the tumor-lymph node-metastasis staging system [9]. The study protocol was approved by the Medical Ethics Committee of our institution on 20 February 2023 (No. K22-396). The requirement for informed consent was waived due to the retrospective nature of the study.
Under general anesthesia and double-lumen intubation, the patients were placed in the right or left lateral decubitus position. All patients underwent uniportal video-assisted thoracoscopic surgery (VATS), which involved making a 3–5-cm incision in the fourth intercostal space between the anterior and middle axillary lines. A wound protector, a 30° thoracoscope, and articulated endoscopic staplers were used in all cases [10].
After dissecting the segmental/subsegmental artery and vein, the segmental/subsegmental bronchus was isolated and ligated at its proximal end using a silk suture (Fig. 1A). The distal bronchus was incised using a pair of scissors, and a central venous catheter was inserted (Fig. 1B). A 50-ml syringe was used to connect the distal end of the central venous catheter. Subsequently, an appropriate amount of air was introduced into the target segment/subsegment via the syringe until the segment/subsegment inflated and the demarcation of the ISP appeared (Fig. 1C) [8]. Then, the target segment/subsegment was dissected using a stapler, an energy device, or both (Fig. 1D). The relevant details of the surgical procedures have been previously described [8].
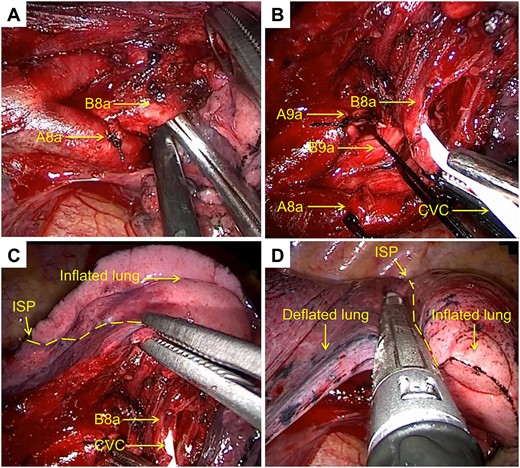
Open insufflation method for left segmentectomy 8a + 9a. (A) Dissection of the subsegmental bronchus (left B8a). (B) Insertion of a central venous catheter at the distal end of the subsegmental bronchus (left B8a). (C) Introduction of an appropriate amount of air into the target subsegment (left S8a) via a 50-ml syringe. (D) Resection of the target lung (inflated) along the intersegmental plane using a stapler.
The surgical margin was evaluated intraoperatively. If the resection margin was <2 cm or the diameter of the resected nodule, additional pulmonary parenchyma resection was performed. Lymphadenectomy was performed if intraoperative frozen sections examination revealed an invasive adenocarcinoma. Air leakage was routinely examined by inflating the residual lung while submerged in water [11]. Obvious air leaks were repaired with sutures. Biological glue or mesh was used in the lung sections to prevent air leaks and bleeding when necessary. At the end of the surgery, a 28-F chest tube was placed through the incision. All the surgeries were performed by the same surgical team.
Patient-controlled analgesia was routinely used, and oral or intravenous analgesics were administered on demand [10]. The chest tube was removed when the lung was fully inflated on chest radiography, there was no evidence of chylothorax, hemothorax, or air leaks, and the drainage was <300 ml daily. The final follow-up date was 21 April 2023.
This study included 41 patients. The median age of the patients was 58 (range 35–73) years, and 63.4% were female individuals. Most (92.7%) patients had no history of smoking. Hypertension was the most common comorbidity. Patients with pulmonary nodules and ground-glass opacities accounted for 92.7% of the total patients. The median diameter of the pulmonary nodules was 0.9 (0.5 − 2.3) cm. Malignant pulmonary nodules accounted for most (80.5%) cases and were staged from 0 to IA2, with histology of adenocarcinoma in situ (36.6%), minimally invasive adenocarcinoma (24.4%), and invasive adenocarcinoma (19.5%).
The surgical procedures are summarized in Table 1. Fourteen patients underwent single subsegmentectomy, 3 underwent single segmentectomy, 12 underwent combined subsegmentectomy, 7 underwent subsegmentectomy combined with segmentectomy, and 5 underwent subsegmentectomy or subsegmentectomy combined with wedge resection.
| Type of RS . | Synchronous procedures . | Number . | Type of LS . | Synchronous procedures . | Number . |
|---|---|---|---|---|---|
| RS1a | 1 | LS1 + 2a | 2 | ||
| RS1 | 2 | LS1 + 2b | RULW | 1 | |
| RS1a + 2 | 3 | LS1 + 2c | 1 | ||
| RS1b + 3b | RLLW | 1 | LS1 + 2b + c | 2 | |
| RS1a + 2 + 3a | 1 | LS1 + 2b + c + 3a | 1 | ||
| RS2a | 1 | LS1 + 2c + 3a | 2 | ||
| RS2b + 3a | 3 | LS1 + 2a + 3c | 1 | ||
| RS2 + 8a | 1 | LS1 + 2a + 3b + c | LLLW | 1 | |
| RS3a | 6 | LS3a | 2 | ||
| RS3a | RMLW, RLLW | 1 | LS3b + c | 1 | |
| RS3 | 1 | LS8a + 9a | 1 | ||
| RS3a + 8a | 1 | LS6 + 8a | 1 | ||
| RS3b | 1 | ||||
| RS6 + 8a | 1 | ||||
| RS8b | RULW | 1 |
| Type of RS . | Synchronous procedures . | Number . | Type of LS . | Synchronous procedures . | Number . |
|---|---|---|---|---|---|
| RS1a | 1 | LS1 + 2a | 2 | ||
| RS1 | 2 | LS1 + 2b | RULW | 1 | |
| RS1a + 2 | 3 | LS1 + 2c | 1 | ||
| RS1b + 3b | RLLW | 1 | LS1 + 2b + c | 2 | |
| RS1a + 2 + 3a | 1 | LS1 + 2b + c + 3a | 1 | ||
| RS2a | 1 | LS1 + 2c + 3a | 2 | ||
| RS2b + 3a | 3 | LS1 + 2a + 3c | 1 | ||
| RS2 + 8a | 1 | LS1 + 2a + 3b + c | LLLW | 1 | |
| RS3a | 6 | LS3a | 2 | ||
| RS3a | RMLW, RLLW | 1 | LS3b + c | 1 | |
| RS3 | 1 | LS8a + 9a | 1 | ||
| RS3a + 8a | 1 | LS6 + 8a | 1 | ||
| RS3b | 1 | ||||
| RS6 + 8a | 1 | ||||
| RS8b | RULW | 1 |
Abbreviations: LLLW, left lower lobe wedge resection; LS, left segmentectomy; RLLW, right lower lobe wedge resection; RMLW, right middle lobe wedge resection; RS, right segmentectomy; RULW, right upper lobe wedge resection.
| Type of RS . | Synchronous procedures . | Number . | Type of LS . | Synchronous procedures . | Number . |
|---|---|---|---|---|---|
| RS1a | 1 | LS1 + 2a | 2 | ||
| RS1 | 2 | LS1 + 2b | RULW | 1 | |
| RS1a + 2 | 3 | LS1 + 2c | 1 | ||
| RS1b + 3b | RLLW | 1 | LS1 + 2b + c | 2 | |
| RS1a + 2 + 3a | 1 | LS1 + 2b + c + 3a | 1 | ||
| RS2a | 1 | LS1 + 2c + 3a | 2 | ||
| RS2b + 3a | 3 | LS1 + 2a + 3c | 1 | ||
| RS2 + 8a | 1 | LS1 + 2a + 3b + c | LLLW | 1 | |
| RS3a | 6 | LS3a | 2 | ||
| RS3a | RMLW, RLLW | 1 | LS3b + c | 1 | |
| RS3 | 1 | LS8a + 9a | 1 | ||
| RS3a + 8a | 1 | LS6 + 8a | 1 | ||
| RS3b | 1 | ||||
| RS6 + 8a | 1 | ||||
| RS8b | RULW | 1 |
| Type of RS . | Synchronous procedures . | Number . | Type of LS . | Synchronous procedures . | Number . |
|---|---|---|---|---|---|
| RS1a | 1 | LS1 + 2a | 2 | ||
| RS1 | 2 | LS1 + 2b | RULW | 1 | |
| RS1a + 2 | 3 | LS1 + 2c | 1 | ||
| RS1b + 3b | RLLW | 1 | LS1 + 2b + c | 2 | |
| RS1a + 2 + 3a | 1 | LS1 + 2b + c + 3a | 1 | ||
| RS2a | 1 | LS1 + 2c + 3a | 2 | ||
| RS2b + 3a | 3 | LS1 + 2a + 3c | 1 | ||
| RS2 + 8a | 1 | LS1 + 2a + 3b + c | LLLW | 1 | |
| RS3a | 6 | LS3a | 2 | ||
| RS3a | RMLW, RLLW | 1 | LS3b + c | 1 | |
| RS3 | 1 | LS8a + 9a | 1 | ||
| RS3a + 8a | 1 | LS6 + 8a | 1 | ||
| RS3b | 1 | ||||
| RS6 + 8a | 1 | ||||
| RS8b | RULW | 1 |
Abbreviations: LLLW, left lower lobe wedge resection; LS, left segmentectomy; RLLW, right lower lobe wedge resection; RMLW, right middle lobe wedge resection; RS, right segmentectomy; RULW, right upper lobe wedge resection.
All patients underwent uniportal VATS segmentectomy without conversion to multiportal VATS, open surgery, or lobectomy. The median operative time was 84 (range 45–194) min, and the median blood loss was 50 (range 10–150) ml. Both the median chest tube duration and postoperative hospital stay were 2 (range 1 − 7) days. The most common postoperative complication was air leakage, with three (9.7%) patients developing an air leak for >3 days and one (2.4%) developing an air leak for >5 days. No deaths occurred within 30 days after surgery. No tumor recurrence was observed at the last follow-up.
Discussion
This study demonstrated acceptable perioperative outcomes, suggesting that the open insufflation method may be feasible and safe for identifying the ISP for segmentectomy or subsegmentectomy in selective patients. In addition, the open insufflation method can be performed in a uniportal VATS by experienced experts.
The operative time in this study was significantly shorter than that in previous studies [11, 12], which supports the claim that this method can reduce the operative time [8]. In addition, the postoperative duration of chest tube placement was significantly shorter than that in previous studies [13], which may be related to the low incidence of postoperative air leaks (2.4%) in our study. According to the literature, prolonged air leakage (> 5 days) is one of the most common complications of segmentectomy, with an incidence of 0–19% [13–15]. There are three possible reasons for the low incidence of air leaks observed in this study. First, staplers were primarily used for ISP dissection. Second, we routinely performed the air leak test using water; suture repair, biological glue, or mesh was routinely used when necessary to minimize the risk of postoperative air leaks. Third, our center is one of the ultra-high-volume thoracic surgical centers in China, which performs > 10 000 major pulmonary resections each year [16]. Therefore, surgeons at our center have more experience in segmentectomy, and the corresponding complication rate may be lower.
However, certain considerations are required when applying this method. First, the prerequisite for successfully applying the open insufflation method is the accurate identification of the vascular structures and bronchus of the target segment; therefore, preoperative three-dimensional computed tomography reconstruction [17, 18] or careful reading of the CT image can help improve the successful implementation of this technique. Second, owing to the low syringe pressure and small central venous catheter diameter, the open insufflation method may be more suitable for small segment resections (e.g. subsegmentectomy). For larger lung segment resections, such as left superior segment resection, the lung may probably not inflate sufficiently. Third, a suitable amount of air should be injected through the catheter. Excessive gas volume may cause the segments that need to be preserved to inflate due to collateral ventilation. Therefore, some authors suggest that using the anatomical data of each segment by CT imaging to calculate the suitable volume of air needed for inflation may help improve the technique [19].
Currently, there is no consensus regarding the optimal ISP method for segmentectomy. Compared with the conventional modified inflation–deflation method [6, 7], the open insufflation method does not require a waiting period, so it may reduce operative time. It is worth mentioning that there is also a technique to identify the ISP without waiting, which involves dissecting the target segmental/subsegmental artery or vein first and then inflating the lung and dissecting the target segmental/subsegmental bronchus within the waiting time [20, 21]. Compared with the indocyanine green fluorescence and selective segmental inflation methods [6, 7], the open insufflation method requires simpler and cheaper equipment and does not require additional medical staff. Moreover, a central venous catheter instead of an injection needle was used for the distal bronchial insertion inflation, so the open insufflation method is safe and will not lead to serious complications such as air embolism.
The main limitation of this study was that no control group was included. In addition, this study was conducted at a single center, which limits its generalizability. Future multicenter randomized controlled studies are warranted to clarify the efficacy and safety of this method, and to further determine the optimal ISP method for segmentectomy.
Conclusion
Our data showed that the open insufflation method may be a simple, time-saving, effective, and safe technique to identify the ISP for segmentectomy in selective patients.
Acknowledgements
We thank Editage (www.editage.com) for English language editing.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
De-identified data is available from the corresponding author upon reasonable request.
References
Author notes
Wei Dai, Na Mei, and Ye Ning contributed equally to this work and should be considered as co-first authors.



