-
PDF
- Split View
-
Views
-
Cite
Cite
Erdo P Sidarta, Elric B Malelak, Robertus A Datusanantyo, Christopher Lauren, Sri Maliawan, Successful reconstruction of severe traumatic scalp defect with exposed bones in a 6-year-old boy: a case report, Journal of Surgical Case Reports, Volume 2024, Issue 1, January 2024, rjad454, https://doi.org/10.1093/jscr/rjad454
Close - Share Icon Share
Abstract
Full-thickness scalp defect reconstruction is considered challenging for the surgeon. The goal of this procedure is to provide coverage of the calvarium. Scalp defect needs thorough and careful planning in reconstruction, not only in choosing the best closure strategy but also in post-operative care. We report a case of successful reconstruction of traumatic severe scalp and bone loss using local scalp flap in a 6-year-old trauma patient. Free flap reconstruction should be considered in such a defect. However, limited resources prevented us to do so. In craniofacial trauma, the plastic surgeon may be involved as an attending physician in facial trauma or assisting in other trauma, especially in defect closure.
Introduction
The scalp is a structure that provides aesthetic structure and secures the cranial bone. The scalp nature makes it prone to laceration because of trauma. Scalp laceration is typically caused by blunt trauma such as fall, hammer blows or even blast, causing a tear in the skin and underlying tissue. The most common scalp laceration separates skin and aponeurotic galea from the pericranium through the loose areolar tissue layer. The blood vessel network supplying the scalp is contained superficial to aponeurosis galea. Understanding this anatomy is essential to successfully stop bleeding or planning procedures requiring blood supply planning such as flap elevation in scalp defect closure [1, 2]. Scalp inelastic property makes reconstruction procedure troublesome when significant soft tissue defect of the scalp is encountered [2]. Full-thickness scalp defect reconstruction is considered challenging for neurosurgeons and plastic surgeons because of the limited mobility of the scalp. The goal of this procedure is to provide coverage of the calvarium to prevent desiccation and infection. Another technique for small defect closure is skin grafting if the vascularized bed is available [3, 4]. We report a case of successful reconstruction of traumatic severe scalp and bone loss using a local scalp flap in a 6-year-old patient.
Case report
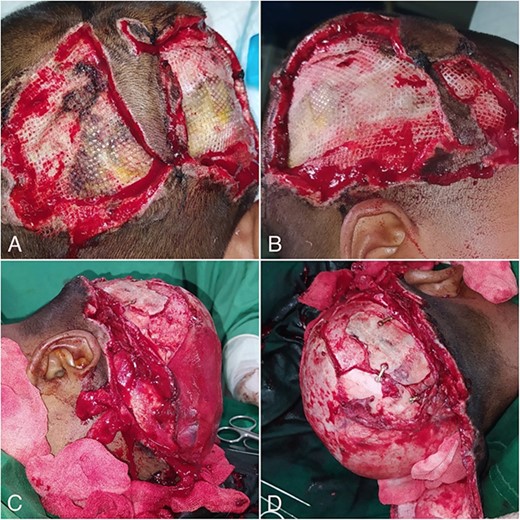
A 6-year-old boy was referred from Belu Hospital in Atambua, about 276 km away, to our hospital with a mild head injury, open scalp wound defect and exposed fractured right temporo-parieto-occipital bone. This patient fell from the motorcycle with her parents after dodging a running wild dog. His head was accidentally squeezed by his father’s body and dragged several metres on the road. The patient was conscious and a 16 × 8 cm defect was observed in the right temporo-parieto-occipital region. We also noticed exposed and depressed fractured bone, some bone loss and a visible dura layer. There was also necrotic tissue in the right parieto-occipital area. The initial physical examination was shown in (Fig. 1).

Initial physical examination showed scalp defect, exposed and depressed fractured bone, some bone loss, visible dura layer and necrotic tissue.
The computed tomography scan confirmed the depressing comminuted fracture of right temporo-parieto-occipital dextra accompanied by subdural pneumocephalus at right fronto-temporo-parieto-occipital, a non-depressed linear fracture of the right frontal bone, right temporoparietal soft tissue loss and multiple petechial intracerebral hematomas at the cortex of right temporoparietal region. We diagnosed this patient with mild brain injury, fractures of the right temporo-parieto-occipital bone and severe scalp defect.
During the surgery, the neurosurgeon removed non-viable bones, decompressed the depressed fracture and debrided non-vital tissue. Fracture bones were secured with mini plates and screws. The neurosurgeon did the craniotomy because of a traumatic brain injury suffered by the patient. Debridement is also done because at the defect a lot of necrotic tissue was found and it was unclean. Placement of plate screw was also done to manage the depressed fracture of the calvaria (Fig. 2).

Pre- and post-debridement, removal of dirty nonviable tissue and decompression of depressed fracture. Some mini plates held the bone fragments securely.
A significant scalp defect in the temporo-parieto-occipital region was closed by the plastic surgeon with a local scalp flap incorporating the left superficial temporal artery (Fig. 3). This procedure was done by making an incision from the fronto-temporal region from right to left. The flap was elevated from the subgaleal layer with a pedicle of the left superficial temporal artery. Split thickness skin was harvested from the right posterior femur to close the secondary defect.
The patients develop no neurological deficit, went home and followed up in the outpatient clinic. Some soft tissue necrosis was observed during the follow-up and left healed by secondary intention (Fig. 4). By 10 weeks postoperatively (Fig. 5), the defects were healed and a monthly visit was encouraged to follow up on any complications. The patient’s parents were satisfied with the result.
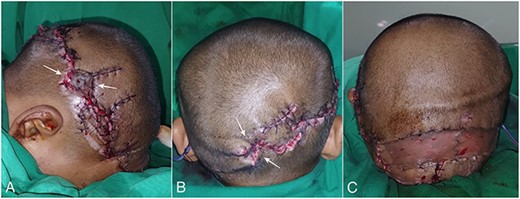
Picture of the post flap (A, B) and skin graft procedure (C). The white arrow showed the necrotic tissue which developed later after the surgery.

Clinical photos 10 weeks postoperatively: frontal view (A), superior view (B), right lateral view (C) and posterior view (D).
Discussion
Large defect of the scalp needs thorough and careful assessment because of their minimal elasticity nature. When scalp and forehead reconstruction is considered, several factors are important in the development of the surgical plan. The factors assessed are size, site, depth of the wound, laxity of the scalp and patient factors such as age and comorbidities. Successful reconstruction of the scalp requires careful preoperative planning, adequate debridement, precise intraoperative execution and proper post-operative care. Primary closure is still the best treatment, treating with the simplest reconstruction should be used whenever possible and also proved to provide the most functional and aesthetic scalp reconstruction. The goals of reconstruction are to restore the scalp with hair-bearing skin by redistribution of local tissue and a good aesthetic outcome [2, 5].
The local scalp flap incorporating the left superficial temporal artery was elevated and transposed to close the bone defect in this patient. Based on the algorithm, free flap reconstruction should be considered in 16 × 8 cm defect [6]. However, limited resources prevented us to do so.
The most common complication of scalp defect reconstruction is bleeding, wound dehiscence, infection, flap necrosis, graft loss and flap loss [5]. We managed the distal flap necrosis and peripheral graft loss by moist wound care and both were healed in secondary intention.
In this case, plastic surgeons were called to assist in defect closure in traumatic head injuries. This was indeed the natural role of plastic surgery. In craniofacial trauma, plastic surgery is involved not only as an attending physician in facial trauma but also as a consulting role in defect closure of neurosurgical trauma. As long as the procedures focus on resection, repair, replacement and reconstruction of defects to restore the form and function of the skin and its underlying anatomic structures, they are considered in the field of plastic surgery [7]. This collaboration should encourage other management of severe head trauma involving scalp defects between neurosurgeons and plastic surgeons elsewhere to achieve a satisfying outcome in a very young patient.
Conflict of interest statement
The authors have no conflicts of interest to disclose.
Funding
No funding.
Data availability
No publicly available datasets were used in the writing of this manuscript.



