-
PDF
- Split View
-
Views
-
Cite
Cite
Weibin Du, Yafeng Mo, Yi Dong, Chun He, Fengzhen Zhou, Fangbing Zhu, The clinical diagnosis and treatment of the shoulder terrible tetrad: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 9, September 2023, rjad499, https://doi.org/10.1093/jscr/rjad499
Close - Share Icon Share
Abstract
Traumatic anterior dislocation of the shoulder is often associated with anterior glenoid fracture or bankart injury. It can also be associated with rotator cuff injury, humeral greater tuberosity fracture, or brachial plexus injury. However, there are few clinical reports of all the above-mentioned injuries at the same time. We report a case of the left “Shoulder terrible tetrad.” After closed reduction of the left shoulder dislocation, we performed one-stage arthroscopic massive rotator cuff repair (Chinese-Way technique) and anchor repair of the bony bankart injury. After 2 years follow-up, the left shoulder function recovered well and the range of motion was satisfactory. A detailed physical examination and electromyography (EMG) examination should be performed in time to avoid misdiagnosis and missed diagnosis, when the clinical manifestation of brachial plexus nerve injury appears after shoulder dislocation. The repairable rotator cuffs tears and bankart injuries can be repaired under shoulder arthroscopy in one stage.
Introduction
Gonzalez et al. [1] first reported the combination of peripheral nerve injury and rotator cuff tear following anterior dislocation of the shoulder in 1991. Michael Marsalli et al. [2] further suggested that the “Shoulder terrible triad” should include: (i) traumatic anterior shoulder dislocation, (ii) rotator cuff tears or displaced humeral greater tuberosity fracture, (iii) brachial plexus injury in 2020. Takase et al. [3] first reported a case of concurrent rotator cuff tear and axillary nerve palsy associated with anterior dislocation of the shoulder and a large glenoid rim fracture, and named it the “Shoulder terrible tetrad” in 2014. There have been a few reported cases of the “terrible tetrad.” We retrospectively analyzed the clinical diagnosis and treatment of a case of the “shoulder terrible tetrad,” and reviewed the literature, hoping to provide reference for the diagnosis and treatment of shoulder joint injury to avoid misdiagnosis and missed diagnosis.
Case presentation
Consent for publication was signed by our patient and approved by the Ethics Committee.
A 56-year-old man, fell from a height while working on 14 November 2020. After treatment in other hospital, left shoulder joint X-ray films were taken, which indicated that the anterior dislocation of left shoulder joint combined with fracture of anterior inferior glenoid joint. The patients were treated with manual closed reduction and fixation in chest position. Then the patient was referred to our hospital for further management. Clinical physical examination found a significant limitation in the range of motion of the left shoulder joint, shoulder stiffness, muscle weakness, and there was sensory disturbance over the lateral aspect of the shoulder (Fig. 1a–d).
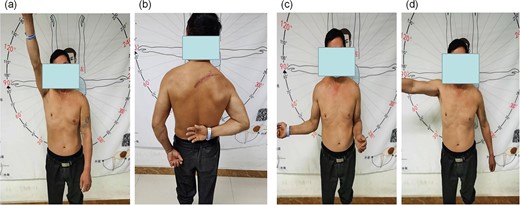
Preoperative functional comparison of both upper limbs: (a) lift of both upper limbs; (b) internal rotation of both upper limbs; (c) external rotation of both upper limbs; (d) abduction of both upper limbs.
Left shoulder joint X-ray, three-dimensional CT (3D CT), and magnetic resonance imaging (MRI) were performed after admission. X-ray and 3D CT scanning revealed an upward shift of the left humeral head, fracture of the anterior inferior glenoid of the left shoulder, and Hill-Sachs injury of the posterolateral left humeral head (Fig. 2a–c). MRI scanning revealed the left humeral head moved up obviously and the subacromial space of the shoulder decreased. The distance between the acromion and humeral head was about 4 cm. The supraspinatus tendon retracted ~4 cm, and the anterior and posterior lacerations were ~4 cm in size. The involved tendons were supraspinatus, infraspinatus, and subscapular, but were not accompanied by significant muscle atrophy and fat infiltration (Fig. 2d–f).
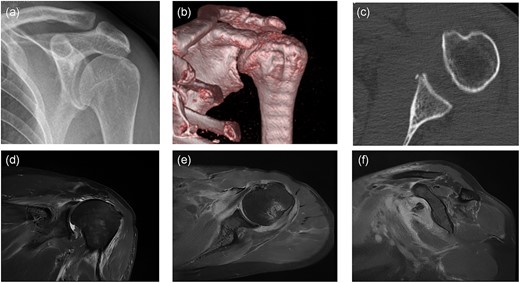
Preoperative imaging: (a) anteroposterior X-ray of the left shoulder; (b) anteroposterior CT 3D reconstruction of the left shoulder; (c) coronal CT radiograph of the left shoulder; (d) anteroposterior MRI of the left shoulder; (e) coronal MRI of the left shoulder; (f) sagittal MRI of the left shoulder.
Electromyography (EMG) and nerve conduction study revealed axillary nerve injury. The preoperative diagnosis was traumatic anterior dislocation of the left shoulder, fracture of the anterior inferior glenoid of the left shoulder (bony bankart injury), massive rotator cuff tear of the left shoulder, and axillary nerve injury.
We performed arthroscopic repair of left shoulder under anesthesia on 20 November. We first used three 2.9 mm anchors to repair the bony bankart injury. Then the subacromial bursa was cleaned and the acromioplasty was performed, the coracoacromial arch was preserved, and a 4.5 mm anchor was used to repair the subacromial tendon in the footprint area of the rotator cuff. Finally, in the Chinese-Way technique, a 4.5 mm anchor was used to move the biceps tendon backward, and supraspinatus and infraspinatus tendons were sutured laterally to the long head of the biceps tendon, respectively, the anterior and posterior supraspinatus tendons and the lateral infraspinatus tendons were fixed with 4.5 mm anchors. Postoperative X-ray and MRI revealed the left humeral head returned to its anatomic position, the rotator cuff tear, and the bony bankart injury had been repaired (Fig. 3a–d).
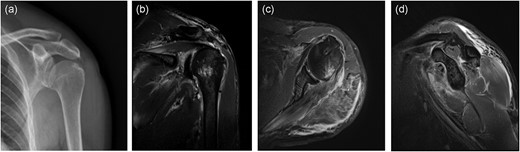
Postoperative imaging: (a) anteroposterior X-ray of the left shoulder; (b) anteroposterior MRI of the left shoulder; (c) coronal MRI of the left shoulder; (d) sagittal MRI of the left shoulder.
The patient continued postoperative treatment with nerve nutrition, shoulder abduction brace immobilization for 6 weeks, complete braking for the first 2 weeks, active movement of the left wrist and elbow joint, followed by passive forward flexion and pendulum exercises in supine position. Six weeks later, passive forward flexion (supine and standing position), pendulum exercises, and passive external rotation were started, and active and passive posterior extension and internal rotation were started in March, followed by gradual return to daily activities. The patient started to be able to exercise vigorously after 6 months. The patient is now 2 years postoperative with good functional recovery of the shoulder joint and generally satisfactory range of motion. Constant score recovered from 38 to 79.
Discussion
Traumatic anterior shoulder dislocation is often associated with anterior glenoid fracture or bankart injury, rotator cuff injury or humeral greater tuberosity fracture or brachial plexus injury (including brachial plexus root, radial nerve, ulnar nerve, median nerve, axillary nerve, musculocutaneous nerve, suprascapular artery nerve). However, there are few clinical reports of all the above-mentioned injuries at the same time [4–7]. Takase et al. [3] first reported and named it the “shoulder terrible tetrad” in 2014. In contrast to the “shoulder terrible tetrad,” there are currently more clinical reports on the “shoulder terrible triad,” which accounts for 9%–18% of all shoulder dislocations [5, 7–10]. However, the exact incidence of “shoulder terrible tetrad” accounting for shoulder dislocation is not known at this time.
Once the diagnosis of the “shoulder terrible tetrad” is clear, the specific clinical treatment plan should be considered according to the degree of combined injury, specific needs, and age of the patient and so on [2, 3]. In this patient, we repaired the massive rotator cuff tear by transposition of the long head tendon of the biceps tendon in one stage, and the postoperative result was satisfactory. However, for irreparable massive rotator cuff tears combined with axillary nerve injury, where rotator cuff muscle atrophy and fatty infiltration have already occurred, it is not recommended to perform complex shoulder reconstruction surgery such as superior capsule reconstruction or reverse shoulder arthroplasty in one stage without knowing the extent of brachial plexus nerve injury, especially axillary nerve injury.
Second, for combined anterior shoulder glenoid complex injuries such as anterior capsular, bankart injury, and bony bankart injury, the degree of displacement of the glenoid fracture, age, and the patient’s needs are critical to the subsequent treatment plan. In young patients with acute bony bankart injury, both rotator cuff tear and bankart injury should be repaired to restore shoulder joint stability in order to better restore shoulder joint function. In this patient, we repaired both the bony bankart injury and the rotator cuff tear, and the postoperative recovery was satisfactory. In the literature, bony bankart injury with fracture displacement of more than 4 mm or involvement of more than 20% of the glenoid is recommended for surgical reduction and fixation [11]. Sang-Jin Shin et al. further concluded that for large rotator cuff tear (>3 cm), repair of the rotator cuff is sufficient to achieve rotator joint stability without considering bankart injury; however, for small to medium rotator cuff tear, repair of both bankart injury and rotator cuff tear is required [12].
Finally, in patients with rotator cuff injury or humeral greater tuberosity fracture, their shoulder joint abduction function is limited, which obviously interferes with the diagnosis of axillary nerve injury. Therefore, after emergency shoulder joint repositioning, if the lateral shoulder joint sensation is impaired or the shoulder cannot be shrugged, nerve injury is highly suspected, and EMG of the upper limb is recommended. In our case, the axillary nerve function recovered completely at 6 months after the injury, and other reports in the literature have similarly found that 87.5%–100% of patients with nerve injuries recover 3–24 months post-injury [13–17]. Therefore, it is particularly important to adequately inform patients with the shoulder terrible tetrad about the long recovery time prior to surgery.
Conclusion
A detailed physical examination and timely EMG examination should be performed to avoid misdiagnosis and missed diagnosis in the diagnosis of the shoulder terrible tetrad. Once the diagnosis is clear, the specific clinical treatment plan should be considered according to the degree of combined injury, specific needs, and age of the patient. For repairable rotator cuff tear and bankart injury, one-stage repair can be performed under shoulder arthroscopy with reliable clinical efficacy.
Author contributions
F.Z. (Fengzhen Zhou) and C.H. contributed to the conception and design of the study. W.D. and Y.M. wrote the manuscript. Y.D. collected the patient's clinical data. F.Z. (Fangbing Zhu) reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest statement
None declared.
Funding
This work is supported by Hangzhou Medical and Health Technology Planning Project (Nos B20200127, B20200203, B20220021), Special Research Project of the Affiliated Hospital of Zhejiang Chinese Medical University (No. 2021FSYYZY43), Zhejiang Province Traditional Chinese Medicine Science and Technology Project (No. 2023ZR046), Hangzhou Agricultural and Social Development Research Guide Project (No. 20220919Y084) which supported us in data collection, analysis, and following up the patients.
Data availability
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study involving human participants was reviewed and approved by Ethics Committee of the Affiliated Jiangnan Hospital of Zhejiang Chinese Medical University (Hangzhou Xiaoshan Hospital of Traditional Chinese Medicine, Approval No. 2020XSZYY12014). The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
Author notes
Weibin Du and Yafeng Mo contributed equally to this paper.
- arthroscopy
- physical examination
- electromyography
- fractures
- brachial plexus
- follow-up
- humerus
- range of motion
- shoulder dislocations
- signs and symptoms
- shoulder region
- rotator cuff injuries
- shoulder dislocations, anterior
- nerve injuries
- brachial plexus injuries
- humerus fractures, greater tuberosity
- misdiagnosis
- rotator cuff repair
- shoulder arthroscopy
- clinical diagnosis
- missed diagnosis



