-
PDF
- Split View
-
Views
-
Cite
Cite
Sivakumaran Gobinath, Sreekanthan Gobishangar, Antony Joseph Thanenthiran, Suntharamoorthy Iyer Thuraisamy Sarma, Jathavani Mario Maznet Theepan, Paramanathan Shathana, Challenging refractory type B lactic acidosis in gastric adenocarcinoma—a successfully managed case, Journal of Surgical Case Reports, Volume 2023, Issue 8, August 2023, rjad412, https://doi.org/10.1093/jscr/rjad412
Close - Share Icon Share
Abstract
Type B lactic acidosis is a rare complication of gastric adenocarcinoma and is associated with poor prognosis. Very few cases have been reported in the literature. A 48-year-old female presented with recurrent episodes of vomiting, loss of appetite and loss of weight for 1 month duration. Endoscopy and subsequent biopsy revealed poorly differentiated adenocarcinoma at the pyloric antrum causing gastric outflow obstruction. Contrast enhanced computed tomography scan of the chest, abdomen and pelvis revealed a malignant neoplasm of the pylorus with no distant metastasis. She developed refractory lactic acidosis not responding to medical treatment. Distal gastrectomy with limited lymph node clearance was done and lactic acidosis improved. Pathophysiology of type B lactic acidosis in solid organ malignancies can be due to the rapid turnover of cells inducing anaerobic glycolysis, thiamine deficiency and extensive hepatic metastasis. This patient did not have hepatic metastasis. This is a successful, surgically managed case of type B lactic acidosis in a patient with gastric adenocarcinoma so far reported in the region. Type B lactic acidosis is very rare in gastric cancer. Patients with refractory lactic acidosis should bring about high suspicion of solid organ malignancies and good clinical outcomes can be obtained by the reduction of tumour burden.
INTRODUCTION
Type B lactic acidosis is defined as non-hypoxia induced lactic acidosis [1]. It is a rare complication of malignancy. It is seen often in haematological malignancies and rarely in solid organ malignancies [2]. Very few cases of type B lactic acidosis in gastric cancers have been reported so far. The exact pathophysiology is not clear. Plausible mechanisms are thiamine deficiency, rapid turnover of malignant cells producing excess pyruvate, Warburg effect and reduced hepatic excretion of lactate as a result of extensive liver metastasis. Here we report a successfully managed case of such a presentation.
CASE PRESENTATION
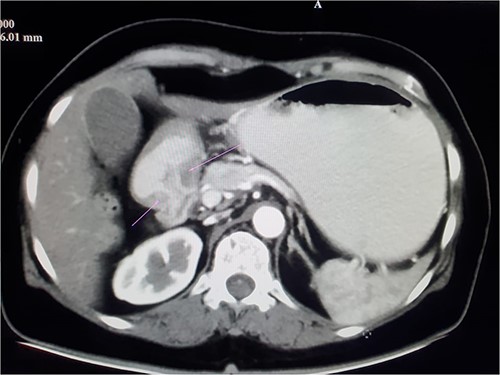
A 48-year-old female who was previously healthy presented with recurrent episodes of vomiting, loss of appetite and loss of weight for 1 month duration. On clinical examination, she was emaciated with a body mass index of 17, not icteric, a vague mass felt over the right hypochondriac region. She was haemodynamically stable. Initial evaluation with gastroscopy showed growth at the pyloric antrum causing gastric outflow obstruction. Biopsy revealed poorly differentiated adenocarcinoma. Contrast enhanced computed tomography (CECT) of the chest abdomen and pelvis showed mucosal thickening seen in the distal lesser curvature, adjacent antrum and pylorus with contrast enhancement suggestive of stomach neoplasm involving pylorus with few tiny regional lymphadenopathies and no distant metastasis (Fig. 1).
On admission, she was severely dehydrated. Biochemical investigations revealed hypokalaemia and an acute kidney injury (K+ 2.7, Creatinine—187). Fluid depletion and electrolyte imbalance were corrected. She was started on parenteral nutrition. On day 3 of admission, she became haemodynamically unstable and collapsed in the ward. Possible causes such as hypovolemic shock, refeeding syndrome and pulmonary embolism were considered.
She was resuscitated with intravenous fluids and managed with broad-spectrum antibiotics, oxygen support and inotropes. Arterial blood gas revealed lactic acidosis (PH =7.332, Lactate—9.9, HCO−3—12.2). She was transferred to Intensive care unit for further monitoring and care. There was no improvement in lactic acidosis noted with resuscitation. Thiamine replacement was given. A CECT abdomen was done to rule out the cause of lactic acidosis that doesn’t show any significant findings except minimum free fluids in the abdomen. Lactate levels were persistently going high. A diagnostic laparoscopy was done that doesn’t show any evidence of bowel ischemia. She was managed with Bicarbonate infusion and renal replacement therapy.
A decision to proceed with surgery was made following a discussion with the multidisciplinary team. She was optimized to the best and a distal gastrectomy with limited lymph node clearance was performed. Following surgery, her lactate levels settled down progressively and she improved clinically within 48 h (Fig. 2). The histology of the resected specimen revealed adenocarcinoma (Fig. 3).
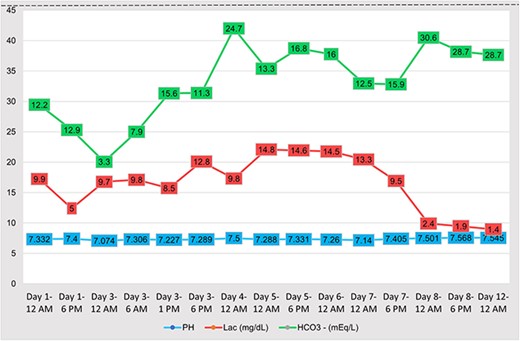
The trend of pH, Lactate and bicarbonate levels in serum samples with time during management.
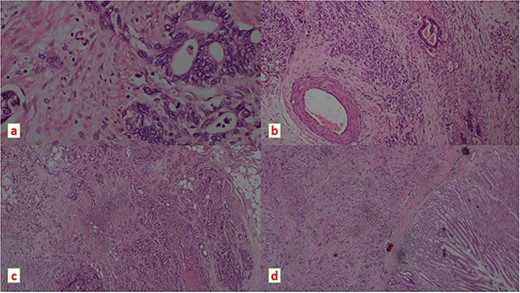
Histopathology images showing moderately differentiated adeno carcinoma on H & E stain under light microscope, (a) magnification ×400 (b) ×100 demonstrating a vascular emboli (c) magnification ×100 demonstrating peri neural invasion (d) magnification ×40.
DISCUSSION
There are many causes for type B lactic acidosis such as liver disease, malignancy, medications such as metformin, treatment with epinephrine, total parenteral nutrition, human immunodeficiency virus infection, thiamine deficiency, mitochondrial myopathy, congenital lactic acidosis, trauma, excessive exercise, diabetic ketoacidosis and ethanol intoxication [1]. A few cases of type B lactic acidosis have been reported in the literature following solid organ malignancies and only two cases with gastric adenocarcinoma [2–4].
Few theories have been proposed to explain the pathophysiology of type B lactic acidosis in solid organ malignancies. Tumour cells with very high turnover rates can induce anaerobic metabolism and enhance pyruvate production. Tumour cells by means of the Warburg effect can do glycolysis even in the presence of oxygen [3].
Malignancy can indirectly cause type B lactic acidosis by thiamine deficiency, especially in the context of rapidly proliferating tumours and patients who get total parenteral nutrition. Thiamine is an essential cofactor for the pyruvate dehydrogenase complex, which converts pyruvate to acetyl-CoA and allows aerobic metabolism to proceed [5].
Malignancies with extensive hepatic metastasis have impaired lactate clearance. Most of the reported solid organ malignancies with type B lactic acidosis have extensive liver metastasis [4]. Out of the two published cases of type B lactic acidosis, both had extensive liver metastasis [3, 4]. But in this case, there was no liver metastasis, and the lactate level has not improved with thiamine replacement as well.
In certain cases, lactate levels improved with the reduction of tumour burden either by chemotherapy or radiation therapy [4, 6]. The surgical reduction was opted for in this patient with a view to reducing the tumour burden and a successful outcome was obtained.
CONCLUSION
Type B lactic acidosis is very rare in gastric cancer. Patients with refractory lactic acidosis should bring about high suspicion of solid organ malignancies and good clinical outcomes can be obtained by the reduction of tumour burden.
ACKNOWLEDGEMENTS
The authors thank the staff of the Histopathology department and the Radiology department, Teaching Hospital Jaffna for helping us with the images.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no conflicts of interest.
FUNDING
The authors received no financial support for this research, authorship and/or publication.
CONSENT
Written informed consent was obtained from the patient for anonymized information and accompanying images to be published in this article. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
DATA AVAILABILITY
The data associated with this study are available upon request.
References
- thiamine deficiency
- computed tomography
- biopsy
- weight reduction
- cancer
- drug clearance
- adenocarcinoma
- endoscopy
- gastric cancer
- acidosis, lactic
- glycolysis
- vomiting
- abdomen
- pyloric stenosis
- gastric outlet obstruction
- lymph nodes
- neoplasms
- pelvis
- pyloric antrum
- pylorus
- chest
- treatment outcome
- liver metastases
- gastric adenocarcinoma
- metastasis, distant
- loss of appetite
- billroth i procedure
- medical management



