-
PDF
- Split View
-
Views
-
Cite
Cite
Ritika Mittal, Aabid Ashraf, Monika Gupta, Mausam Shah, Scar endometriosis: the menace of surgery, Journal of Surgical Case Reports, Volume 2023, Issue 7, July 2023, rjad413, https://doi.org/10.1093/jscr/rjad413
Close - Share Icon Share
Abstract
Caesarean scar endometriosis (CSE) is a rare type of abdominal wall endometriosis and is frequently missed on initial presentation. A case of CSE diagnosed and treated by surgical excision is presented. Although rare, CSE should be considered a possibility in the differential diagnoses of pain and mass at scar site.
INTRODUCTION
Endometriosis is a benign disorder, predominantly seen in women of reproductive age, where in the endometrial components are found outside the uterine cavity [1]. The most common locations are pelvic, however, uncommonly, extra pelvic endometriosis has also been reported. One of the rare sites is the abdominal wall. Abdominal wall endometriosis (AWE) mostly tends to occur at previous surgical scars, usually following gynaecological and obstetric procedures with reported incidence of ˂1%. Diagnosis of caesarean scar endometriosis (CSE) is challenging due to rarity of the condition and the relative lack of awareness amongst the clinicians. We report a case of caesarean section scar endometriosis.
CASE REPORT
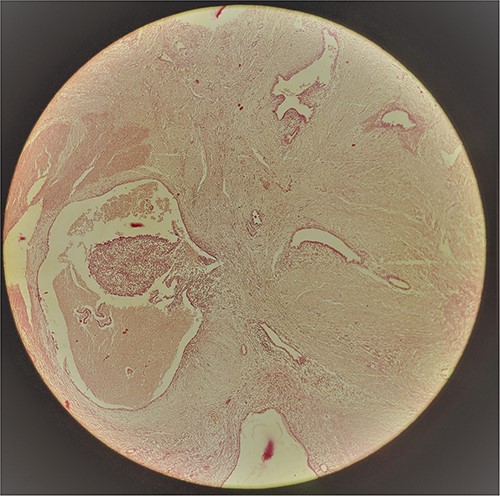
A 29-year-old female patient presented with a complaint of pain in lower abdomen for last 2 years. The pain would aggravate during menses. She also complained of a swelling at the site of her previous lower segment caesarean section (LSCS) scar for 1 year, which had gradually increased in size. She had underwent LSCS two and half years back. Nothing else was significant in history. Examination revealed a well circumscribed, firm mass at the surgical scar site, slightly to the right of the midline, ⁓6 cm × 5 cm in dimensions, fixed to underlying structures, especially on contraction of the rectus abdominis. Ultrasonography showed a heterogenous mass in the relation to the scar. Magnetic resonance imaging (MRI) revealed a well-defined heterogenous lesion extending into right rectus abdominus muscle, 4.2*3.1*2.2 cm in size with multiple thin septations within it, suggestive of scar endometriosis. Intraoperatively an irregular mass lesion was found in the subcutaneous scar tissue and was noted to be invading the rectus abdominis (Fig. 1). Enbloc excision of the endometrioma along with the involved portion of rectus sheath and rectus abdominis muscle was done (Figs 2 and 3). In view of potential tension on the fascial closure onlay mesh reinforcement was also done. The post operative course was uneventful and the patient was discharged on 7th post operative day. The histopathological examination confirmed the presence of endometrial tissue within the excised mass with skeletal muscle bundles infiltrated by endometrial glands (Fig. 3). Patient is on regular follow up and is recurrence free at 9 months.
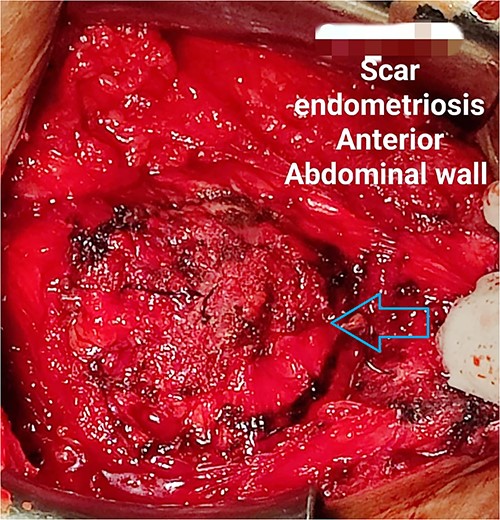
Anterior aspect of the endometrioma (pointed out by the arrow) delineated after dissection of skin flap.

The cut section revealing areas of haemorrhage, pointed out by the arrow.
DISCUSSION
AWE is uncommon. Though it can occur spontaneously but is usually seen following gynaecological and obstetric procedures, like caesarean section [2]. And as expected the most common type of AWE is CSE. The incidence rates reported in literature vary widely, usually ˂1% [2], as most of the data is derived from case reports or series. The condition frequently follows caesarean section. The pathogenesis of CSE appears to be complex; however, the most widely accepted theory is the Implantation Theory, suggesting that endometriosis results from direct inoculation of endometrial cells into the wound during the surgical procedure followed by oestrogen driven growth [3]. Some reports have speculated a higher risk of endometriosis with Pfannenstiel incision than a midline vertical incision, however the evidence is insufficient [4]. Presentation may vary with pain and/or mass being the most common features reported in up to 80% cases [5]. The triad of a palpable tumour, cyclic pain and a history of caesarean section, called the Esquivel triad is almost diagnostic of AWE [6]. A cyclical pattern of pain with worsening during menstruation provides a valuable clue to diagnosis. The time interval between the index surgery and the manifestation varies and in this patient was 6 months. Ultrasonography is the initial imaging modality employed. The characteristic appearance on ultrasonography is of a hyperechoic solid lesion with internal vascularity. Cross sectional imaging may be diagnostic, with MRI better than computed tomography in terms of resolution and soft tissue delineation [7]. Fine needle aspiration cytology (FNAC) is difficult to interpret in scar endometriosis and involves the possibility of needle track implantation [8]. Histopathology provides the definitive diagnosis and presence of endometrial glands, stroma or hemosiderin containing macrophages is diagnostic. Hernia, haematoma, lipoma, desmoids, metastatic tumours are the usual differentials. The management is primarily surgical but medical treatment with progesterone, antioestrogens such as danazol, and gonadotropic agonists like leuprolide acetate has been tried with poor success [9]. Excision with wide margins is critical to prevent recurrence. Invasion into muscles or aponeurosis warrants enbloc excision and a residual defect may need reinforcement with prosthetic mesh as was needed in this patient. Several protective measures like vigorous flushing of the wound cavity, obliteration of dead space have been suggested as strategies to decrease the incidence of CSE.
CONCLUSION
CSE may be more common than presumed given the sheer volume of caesarean sections being performed and should be considered in all women of reproductive age presenting with pain and mass at the scar site. Awareness as regards the possibility of the condition is imperative to avoid delays in management. Management is primarily surgical with attention warranted towards fascial strength and need for reconstruction.
AUTHORS’ CONTRIBUTIONS
All the authors have contributed to the concept, writing, editing of this manuscript.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
Data is available on request from the corresponding author.



