-
PDF
- Split View
-
Views
-
Cite
Cite
Yi-Sheng Shih, Yao-Jen Chang, Yu-Ting Cheng, Chia-Sung Chang, Yu-Hsien Lin, Flexor pollicis longus tendon rupture: a case series on palmaris longus tendon graft reconstruction after volar plate fixation, Journal of Surgical Case Reports, Volume 2023, Issue 7, July 2023, rjad399, https://doi.org/10.1093/jscr/rjad399
Close - Share Icon Share
Abstract
Flexor pollicis longus (FPL) tendon rupture is a debilitating condition that can impair hand function. This case series study aimed to evaluate the outcomes of FPL tendon rupture and subsequent palmaris longus (PL) tendon graft reconstruction. Three cases of FPL tendon rupture in patients who had previously undergone open reduction and internal fixation with a volar plate were included. The surgical intervention involved volar plate removal, tenolysis and PL tendon graft reconstruction. Follow-up assessments showed gradual improvement in wrist function, with no post-operative complications or infections observed. These findings suggest that PL tendon grafting can be an effective surgical technique for FPL tendon rupture. Further research is needed to determine optimal surgical approaches and post-operative rehabilitation protocols for this condition.
INTRODUCTION
Flexor pollicis longus (FPL) tendon rupture is a relatively uncommon but debilitating condition that can severely impair hand function [1]. It is frequently caused by wrist trauma or repetitive activities that exert excessive strain on the tendon [2]. Conservative treatment, including immobilization and physical therapy, may be successful in some cases, but surgical intervention is often necessary to restore function [3]. Volar plate fixation of distal radius fractures is a common surgical technique that may cause FPL tendon rupture [4]. One of the most popular surgical methods for FPL tendon rupture is tendon grafting, in which a graft from the palmaris longus (PL) tendon is used to reconstruct the FPL tendon [5]. Despite the effectiveness of tendon grafting, there is still uncertainty about the optimal surgical technique and post-operative rehabilitation protocol [6]. Furthermore, there is limited data available on long-term outcomes and complications linked with FPL tendon rupture and tendon grafting [7]. Therefore, we present a case series of FPL tendon ruptures that underwent PL tendon grafts for reconstruction, with a specific emphasis on surgical technique, rehabilitation and outcomes.
This case series aims to offer a comprehensive review of the current literature on FPL tendon rupture and tendon grafting, including volar plate induced FPL tendon rupture and PL graft for reconstruction, as well as to contribute to the ongoing discussion on optimal management strategies for this condition.
METHOD
Our clinical study is a case series conducted at a single center in Taiwan, covering the period from 1 January 2021 to 31 December 2022. The study focuses on patients who underwent previous open reduction and internal fixation (ORIF) with volar plate and subsequently suffered from FPL tendon rupture, resulting in volar plate removal and PL tendon graft.
CASE PRESENTATION
Case 1
A 61-year-old male who denied any systemic disease, with a past medical history of a left distal radial fracture, which was treated with ORIF with a plate on 29 January 2017. He presented to the plastic surgery Outpatient Department (OPD) in July 2020 with a protruding mass over his left palmar wrist, which had been causing him pain for the past 3 weeks. On examination, poor flexion of the left thumb was noted. Upon suspicion of a ruptured FPL tendon, a sonogram was arranged, which confirmed the diagnosis (Fig. 1). After discussion with the patient, it was decided that he would undergo surgery.
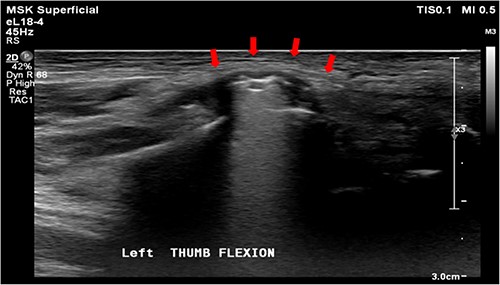
Sonogram of the left wrist showing a ruptured FPL tendon. The arrow points to the discontinuity in the tendon, indicating the site of rupture.
He was admitted to the hospital for further management and underwent plate removal, tenolysis and tendon graft reconstruction on 19 January 2021 (Fig. 2). The operation was successful, and the patient tolerated it well. No post-operative complications were observed. After the surgery, he was prescribed acetaminophen 500 mg four times a day and morphine 5 mg intramuscularly every 4 h as needed for pain control. Wound care with a wound dressing of Biomycin was also prescribed, and his vital signs and wound condition were closely monitored. Infection prevention was done with Cefazolin 1 g intravenously every 8 h.
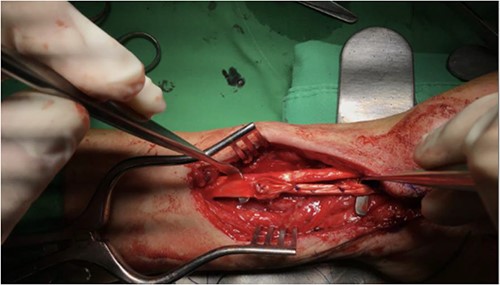
The patient underwent plate removal, tenolysis and tendon graft reconstruction on 19 January 2021.
He was discharged on 21 January 2021, in a relatively stable condition and continued to attend follow-up appointments at the Rehabilitation OPD until 9 November 2022. During this period, he reported gradual improvement in his left wrist function and was satisfied with the outcome of the surgery. Physical examination revealed that the range of motion in his left wrist had significantly increased compared to before the operation. There were no signs of infection or wound complications noted during the follow-up visits.
Case 2
A 68-year-old female with underlying diseases of dyslipidemia, hypertension and a history of left distal radial fracture status post open reduction internal fixation on 4 April 2021, presented to our plastic surgery OPD on October 2022 with complaints of limited left thumb flexion for the past month. She reported experiencing sudden pain in her left forearm and left wrist radial site while pulling grass at home. On examination, she was found to have poor flexion of the left thumb, which was suggestive of a rupture of the FPL tendon. Left wrist X-ray showed fracture over radius with compression plate fixation (Fig. 3). After thorough discussion with the patient, it was decided that she would undergo tendon repair surgery.
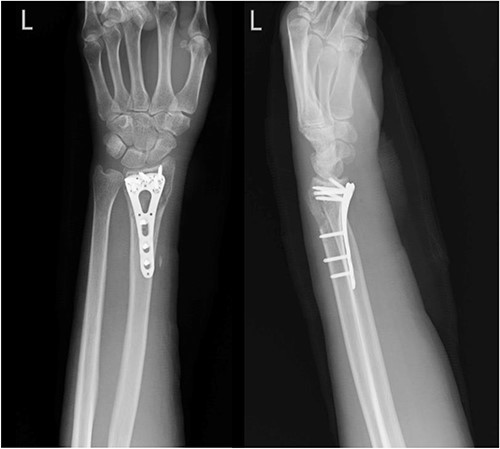
Left wrist X-ray showing a fracture over the radius with compression plate fixation.
Pre-operative assessment was performed, and remove volar plate, tenolysis, release of flexor retinaculum and tendon graft reconstruction of FPL were performed on 1 November 2022, due to total severance with adhesion and fibrosis (Fig. 4). Post-operative pain control was given, and wound dressing was changed regularly. No fever or wound dehiscence was noted during her hospital stay. A rehabilitation specialist was consulted for a spica splint, and the Penrose drain was removed on 3 November 2022. She was discharged on 3 November 2022, in stable condition.

Post-operative photo showing removal of volar plate, tenolysis, release of flexor retinaculum and tendon graft reconstruction of FPL that were performed on 1 November 2022.
During the follow-up appointments at the rehabilitation OPD, which ended on 3 May 2023, the patient reported gradual improvement in her left thumb flexion and was satisfied with the outcome of the surgery. Physical examination revealed that the function of the second to fifth finger was not impaired, and there were no signs of infection or wound complications.
Case 3
A 35-year-old male with no significant medical history fell from a third-floor balcony while working in February 2022, resulting in a right distal radius fracture that was treated with volar plate fixation. However, during an outpatient visit in November 2022, he reported a right thumb weakness that had been present for 3–4 months. Right wrist X-ray showed fracture at distal radius and carpal bones, s/p internal fixation (Fig. 5). A sonogram revealed a right thumb flexor tendon injury (Fig. 6), and he was admitted to our orthopedic ward for surgical repair of the FPL rupture on 12 November 2022. During the operation, plastic surgeon was consulted to repair the FPL rupture with a PL graft, repair the radial artery rupture and vessel with graft, repair the carpal ligament with left tensor fascia lata, release scar contracture of the volar and dorsal carpal region, and perform neurolysis of the median nerve due to adhesion to the FPL tendon.
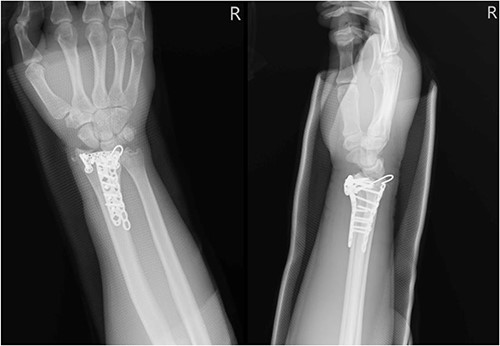
Right wrist X-ray showing a fracture located at the distal radius and carpal bones, which was surgically treated with internal fixation.
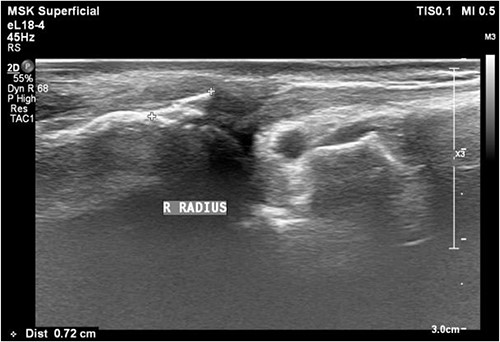
Sonogram of the right thumb showing an injured flexor tendon. Asymmetric fibrillar structures of the right FPL tendon were observed.
Rehabilitation began on 1 December 2022, and during OPD follow-up, the patient reported a gradual improvement in his left wrist function and was satisfied with the outcome of the surgery. On physical examination, the range of motion in his left wrist had significantly increased compared to before the operation.
DISCUSSION
FPL tendon rupture is a known complication after distal radius fracture fixation with volar plate osteosynthesis [8]. The prevalence of FPL rupture following volar plating of distal radius fractures has been reported to range from 0.7% to 10% [8, 9]. The FPL tendon is at risk of injury due to the close proximity to the plate and the potential for impingement or rubbing of the tendon against the hardware. Additionally, the tension placed on the FPL tendon during wrist motion may also contribute to the risk of rupture.
There is ongoing debate regarding whether previous ORIF with volar plate increases the risk of FPL rupture compared to non-operative treatment or other forms of operative fixation [10, 11]. Some studies have found no significant difference in the incidence of FPL rupture between ORIF with volar plate and other forms of operative treatment [12, 13]. However, a systematic review by Grünert and Hahn found that ORIF with volar plate was associated with a significantly higher risk of FPL rupture compared to non-operative treatment or other operative fixation methods [9]. The authors suggested that the location of the volar plate and the amount of stress on the FPL tendon may contribute to the increased risk of rupture.
Plate removal with subsequent FPL tendon repair is the recommended treatment for FPL rupture following ORIF with volar plate [14]. The optimal timing for plate removal is a matter of debate. Some studies suggest that early plate removal, within the first 6–12 months after initial fixation, may reduce the risk of FPL rupture and improve post-operative outcomes [15, 16]. However, other studies have found no significant difference in FPL rupture rates or post-operative outcomes between early and late plate removal [8, 17]. The choice of graft for FPL tendon repair is also a topic of discussion. While autogenous PL tendon graft remains the most commonly used graft, alternative grafts such as extensor indicis proprius and flexor carpi radialis tendons have also been reported [18, 19]. The choice of graft should be based on the surgeon’s experience, patient factors such as age and activity level, and the condition of the available tendons.
Post-operative care following FPL tendon repair involves immobilization of the wrist and hand to protect the repaired tendon, followed by a gradual progression of motion and strengthening exercises [20]. The duration of immobilization and the timing of rehabilitation vary among different studies and should be individualized based on the patient’s progress and the surgeon’s preference. Long-term outcomes following FPL tendon repair are generally favorable, with most patients achieving good functional outcomes and a return to their pre-injury activity level [21, 22]. However, complications such as adhesion formation, delayed or non-union of the graft and recurrence of tendon rupture may occur [23, 24].
In conclusion, FPL tendon rupture is a potential complication following ORIF with volar plate fixation for distal radius fractures, and the optimal treatment strategy remains controversial. However, our case series of three patients who underwent surgical treatment for FPL tendon rupture following distal radius fracture fixation with volar plate osteosynthesis showed favorable outcomes with plate removal and subsequent FPL tendon repair using autogenous PL tendon graft. Post-operative care was individualized, and all three patients achieved satisfactory functional outcomes with a return to their pre-injury activity level, without any observed complications during the follow-up period. Despite the need for further studies with larger sample sizes and longer follow-up periods, our findings suggest that plate removal with subsequent FPL tendon repair using autogenous PL tendon graft may be an effective treatment strategy for FPL tendon rupture following volar plate fixation for distal radius fractures.
ACKNOWLEDGEMENTS
We would like to thank two anonymous reviewers and the editor for their comments.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
- postoperative complications
- follow-up
- reconstructive surgical procedures
- surgical procedures, operative
- tendon injuries
- wrist
- infections
- open reduction with internal fixation
- hand function
- flexor pollicis longus muscle
- palmaris longus muscle
- postoperative rehabilitation
- volar plate
- tendon transplantation



