-
PDF
- Split View
-
Views
-
Cite
Cite
Maha El Maati, Zakia Berjaou, Zaineb Hammouch, Kenza Khachani, Iliass Moustakbal, Meryem Meziane, Nadia Ismaili, Laila Benzekri, Sara Aoufi, Samir Mazouz, Karima Senouci, Surgical management of deep dermatophytosis in a patient with CARD9 deficiency, Journal of Surgical Case Reports, Volume 2023, Issue 7, July 2023, rjad388, https://doi.org/10.1093/jscr/rjad388
Close - Share Icon Share
Abstract
Deep dermatophytosis is a dermal infection caused by Dermatophytes. It can cause deeper dermal dermatophytosis, Majocchi’s granuloma, dermatophytic pseudomycetoma or a widespread infection. CARD9 deficiency is a known risk factor in the Mediterranean region, first reported in 1964 in Morocco. We report a case of 23-year-old man with a scarring alopecia who presented with subcutaneous abscesses topped off with a large ringworm infection. Mycotic analysis revealed a Trichophyton Rubrum deep dermatophytosis. The molecular study revealed a CARD9 mutation confirming dermatophytosis with parotid and lymph nodes involvement. The patient underwent successful drainage surgery of the abscesses alongside medical treatment including antifungal agents and he was discharged after an uneventful postoperative course.
INTRODUCTION
Dermatophytosis disease is an invasion of the dermal and subcutis tissues with dermatophytes causing four types of clinical presentations: deeper dermal dermatophytosis, Majocchi’s granuloma, dermatophytic pseudomycetoma or a widespread infection. CARD9 deficiency is a known risk factor in the Mediterranean region. The first Moroccan case was reported in 1964.
Treatment guidelines are unclear and surgical management can be proposed for recalcitrant cases. We report a case of deep dermatophytic disease that was treated surgically.
CASE REPORT
A 23-year-old man of North African origin, born from a consanguineous marriage, with a history of tinea since childhood, was admitted in the dermatology department for the exploration of multiple subcutaneous abscesses.
Initial physical examination showed multiple subcutaneous formations in the trunk, the scalp associated with ringworm of the glabrous skin (Fig. 1), and a scarring alopecia (Fig. 2) without nail involvement. Inflammatory lymph nodes were found in the cervical and axillary areas. There was no hepatomegaly, abdominal tenderness or ascites.

Subcutaneous abscesses with a ringworm of the trunk; (A) ventral view; (B) and (C) dorsal view.

Ultrasound showed liquid formations containing calcifications among necrotic inflammatory nodes and parotid infiltration.
Mycological analysis revealed the presence of Trichophyton rubrum in the pus and Microsporum canis in the superficial scales (Fig. 3). Microscopy of purulence sampling from intact nodules demonstrated abundant septate hyphae with periodic acid–Schiff and Gomori-Grocott stainings, confirming the diagnosis of deep dermatophytosis (Fig. 4). Molecular study then revealed a CARD9 mutation inducing immunotolerance to fungal infections.
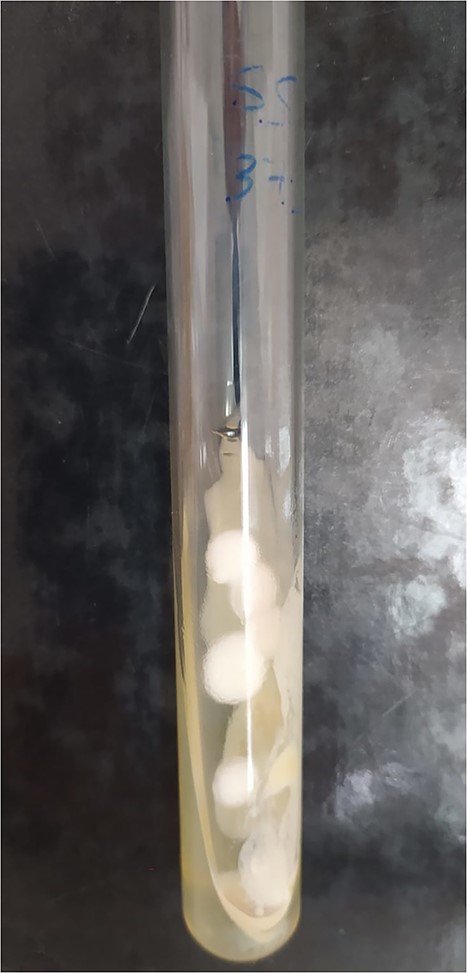
Culture tube for the identification of Trichophyton Rubrum colonies.
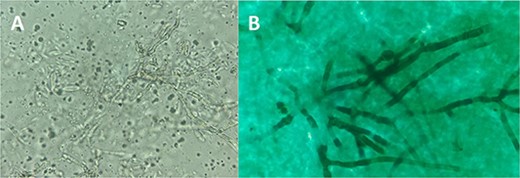
Microscopic examination of pus sample from intact nodules; (A) Fresh microscopic examination at 40× magnification showing abundant septate mycelium hyphae with multiple microconidia; (B) Gomori-Grocott’s methenamine silver staining showed black fungi on a pale green background, confirming the diagnosis of deep dermatophytosis.
Griseofulvin was prescribed at the dose of 1 g per day.
Faced with the multitude and bulkiness of abscesses in the trunk and scalp, as well as the functional discomfort they caused, surgical drainage was proposed.
The patient went under general anesthesia, initially in the supine position. The anterior abscesses were drained with a Delbet blade in place. The patient was then placed in a prone position with removal of the dorsal and scalp abscesses.
The evacuation fluid was creamy with the existence of several septate abscesses (Fig. 5).

The Delbet blades were removed 7 days after the surgery (Fig. 6).

Healing was obtained on the fifteenth day with removal of the sutures.
DISCUSSION
Sequeira may have described the first case of deep dermatophytosis in 1912 [1]. A total of 47 years later, Hadida and Shousboe studied the clinical characteristics of what they referred to as “dermatophytic disease” and documented further cases in 1959 [2].
Rollier described the first case in Morocco in 1964 [1]. Deep dermatophytosis is characterized by dermatophyte infection of the dermis, subcutis and internal viscera. It mostly occurs in the Mediterranean region [3].
Lanternier et al. revealed CARD9 deficiency in relation with dermatophyte infection in 2013, and 24 individuals with infections caused by pathogens of the Trichophyton and Microsporum species were documented so far (6).
CARD9 is an intracellular adaptor protein and mediates antifungal immunity by forming a complex with BCL10 and MALT1, which are key molecules connecting innate receptors to adaptive immune responses, particularly Th1 and Th17 responses [4]. Both congenital and acquired defects at any site(s) along this route weaken host defense, resulting in cutaneous and subcutaneous mycoses.
Tichophyton Violaceum is the most common pathogen, involved in 59.4% of cases. Other species such as Trichophyton schoenleinii, Trichophyton Rubrum and Microsporum Canis have also been identified [3].
However, in immunocompromised individuals or patients with CARD9 gene mutations, Dermatophytes penetrate deeply into the dermis causing deep dermatophytosis [5–8].
Appearing during early childhood [3, 9], lesions frequently begin as recurrent scalp ringworms (51, 7%), tinea corporis (41, 4%) or onychomycosis (6, 8%) [3]. The evolution is then marked by subcutaneous extension of nodules of various sizes mimicking cutaneous tuberculosis as the illness progresses [3].
There are no guidelines on the management of deep dermatophytosis. In extreme cases, the infection becomes life threatening by progressing to the viscera [10–13]. Alopecia is common and can lead to complete hair loss as in our patient.
Improvement of immune status in combination with antifungal agents may be the best therapy. Griseofulvin is the most commonly administered antifungal drug often combined with local treatments. It is prescribed at a dose of 1 g/d. However, more recent molecules such as terbinafine, fluconazole and itraconazole have proven to be more effective but much more expensive. But as in our case, antifungal drugs, even the most recent ones, are not sufficient on their own to obtain a complete healing.
Indeed, an intervention on the immunity is essential and for this reason the association between interferon gamma and antifungal drugs remains the best therapeutic option, even though it is quite expensive. Since the antifungal treatment must be maintained for several years, hepatic monitoring is essential because of the hepatotoxicity of these molecules.
Surgical treatment can be proposed in particularly severe cases due to poor diffusion of the antifungal agents in the collected abscesses, discomfort and esthetics.
The first surgical case was reported in 1977 (9), since then, four patients underwent a surgical procedure (14, 15), three for skin tumors and one for cerebral localization (3).
In all cases reported so far, evolution after surgery follows a favorable course.
Dermatophytic disease not only affects the social life of patients because of the displaying lesions, but also the vital prognosis because of the inexorable evolution toward deep and visceral damage.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
CONSENT
The patient consented to his case to be published in the scientific literature.
DATA AVAILABILITY
All data underlying the results are available as part of the article and no additional source data are required.



