-
PDF
- Split View
-
Views
-
Cite
Cite
Timon Mac Sseruwagi, Catherine R Lewis, Rectal prolapse associated with intussusception and malignancy, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad363, https://doi.org/10.1093/jscr/rjad363
Close - Share Icon Share
Abstract
Rectal prolapse associated with intussusception is when the intestine slides into the adjacent part causing a protrusion through the anus. It is also referred to as recto-anal intussusception or trans-anal protrusion of intussusception. Pre-operative diagnosis of the associated intussusception is usually hard to make. We present a case of a patient who presented with a rectal prolapse. Surgical exploration also noted an intussusception and rectal malignancy. We demonstrate the importance of surgical management in patients with rectal prolapse to avoid progression of a malignancy or intussusception.
INTRODUCTION
The invagination of small bowel was first described by Paul Barbette of Amsterdam in 1674. The term intussusception was later described in detail by John Hunter in 1789. Intussusception is an invagination of a proximal loop of bowel (intussusceptum) into an adjacent distal segment (intussuscipiens). It is more common in children. Intussusception in adults accounts for 5% of all intussusceptions and ~1% of all bowel obstructions [1, 2].
Rectal prolapse is a condition where the rectum protrudes out of the anus. It was first described on papyrus in 1500 BC. In 1912, Moschowitz describes rectal prolapse as a sliding hernia in which the anterior rectal wall herniates through a defect in the pelvic fascia. Beginning in 1968, it was proposed that rectal intussusception was the cause of rectal prolapse. Rectal mucosa 6–8 cm from the anal verge becomes the lead point for the intussusception. It is more common in elderly females [3].
Colorectal carcinoma is a common malignancy worldwide. Primary malignancy is the most common cause of colo-colic intussusception. Rectal prolapse with associated colorectal carcinoma is rare. Neoplasms can function as lead points of intussusception leading to rectal prolapse [4]. Herein, we present a case of a male patient presenting with rectal prolapse with associated intussusception and rectal adenocarcinoma.
CASE PRESENTATION
A 60-year-old male presented with a protruding anal mass of 8 months duration. The mass initially would spontaneously reduce. The mass required manual reduction for the past 2 months. The patient noted fecal incontinence with protrusion of the mass with bowel movements. There was no rectal bleeding reported. The patient reported no significant past medical history. On physical examination, vital signs were within normal limits. There was no evidence of jaundice, pallor, edema or lymphadenopathy. The abdomen was nontender with normoactive bowel sounds. Rectal examination was significant for protrusion of ~6 cm of bowel. There was a central area of ulceration noted without any bleeding (Fig. 1).

Preoperative image: preoperative photograph of full-thickness rectal prolapse with area of ulceration.
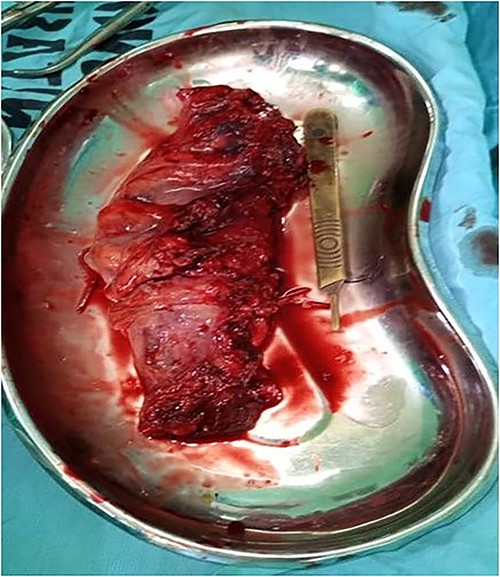
After discussing all surgical options, informed consent was obtained for Altemeier’s procedure. An ~15 cm portion of the rectum was excised (Fig. 2). Upon further evaluation of the gross specimen, there was noted to be an area of intussusception containing a rectal tumor (Fig. 3). The surgical procedure was uneventful, and the patient was discharged on postoperative Day 2.
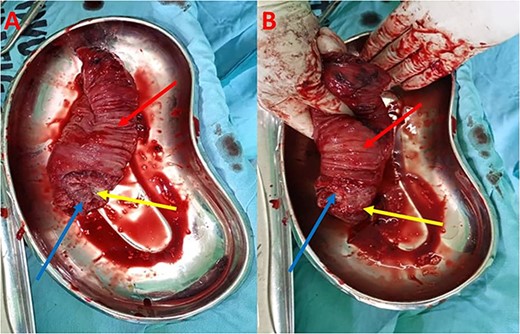
(A) Gross specimen demonstrating intussusception with rectal tumor; (B) Gross specimen demonstrating reduction of the intussusception; red arrow—intussuscipiens; blue arrow—intussusceptum; yellow arrow—rectal tumor.
Histological diagnosis demonstrated an 18 cm segment of colon with a firm mass located 4.5 cm from the distal end. The proximal end of the resection margin had tumor involvement. There was thickening of the intestinal wall and the mass involved the muscularis mucosa. There were sheets and nests of malignant glands diffusely infiltrating the tumor with lymphovascular invasion. Pathological diagnosis was indicative of well-differentiated adenocarcinoma of the rectum. Given the pathological diagnosis, the patient was contacted for a possible abdominal perineal resection for complete oncologic resection. Due to financial constraints, the patient declined further treatment and was lost to follow-up.
DISCUSSION
Rectal prolapse associated with intussusception is also known as trans-anal protrusion of intussusception, internal intussusception, occult rectal prolapse or recto-anal intussusception (RI). RI is present in 12–31% of patients with defecation disorders and is also present in 45–80% of patients with solitary rectal ulcer syndrome (SRUS). SRUS occurs due to forceful straining or because of traumatic injury from the intussusception on the rectal mucosa [5]. This may explain the ulceration present during initial physical examination in our patient.
Trans-anal protrusion of intussusception or RI is a rare complication of intussusception in which the apex of the intussusception is exteriorized through the anus [6]. Patients with trans-anal protrusion of intussusception may be asymptomatic. However, patients may also present with constipation, incomplete evacuation, outlet obstruction that is not relieved with straining, or incontinence. RI can be graded into five categories as indicated in Table 1 [5]. Our patient presented with grade V full-thickness rectal prolapse.
| Grade . | Presenting features . |
|---|---|
| I | No relaxation of the sphincter mechanism |
| II | Mild intussusception |
| III | Moderate intussusception |
| IV | Severe intussusception |
| V | Rectal prolapse |
| Grade . | Presenting features . |
|---|---|
| I | No relaxation of the sphincter mechanism |
| II | Mild intussusception |
| III | Moderate intussusception |
| IV | Severe intussusception |
| V | Rectal prolapse |
| Grade . | Presenting features . |
|---|---|
| I | No relaxation of the sphincter mechanism |
| II | Mild intussusception |
| III | Moderate intussusception |
| IV | Severe intussusception |
| V | Rectal prolapse |
| Grade . | Presenting features . |
|---|---|
| I | No relaxation of the sphincter mechanism |
| II | Mild intussusception |
| III | Moderate intussusception |
| IV | Severe intussusception |
| V | Rectal prolapse |
Defecography is the gold standard in the diagnosis of RI. It involves the injection of contrast into the rectum, followed by fluoroscopy with the patient evacuating the rectal contents while sitting in an upright position on a radiolucent commode. Anoscopy and/or proctoscopy may also be useful to determine viability of the mucosa [7]. Ultrasonography may show a ‘target sign’ in the transverse view or the ‘pseudo-kidney sign’ on the longitudinal view. Computed tomography is the imaging of choice in adults with intussusception, demonstrating a bowel within the bowel appearance [1]. Due to lack of resources and the initial diagnosis of just a rectal prolapse, imaging was not performed in our patient.
Treatment of RI is determined by the underlying symptomatology. Medical management consisting of laxatives, suppositories or enemas is not useful or may cause worsening symptoms. Electromyogram-based biofeedback is first-line treatment for symptomatic RI. Trans-anal Delorme (mucosal proctectomy), Altemeier’s procedure (perineal rectosigmoidectomy) and abdominal rectopexy are surgical options [5].
Intussusception is rare in adults and is caused by benign or malignant tumors in up to 90% of patients. Unlike intussusception in children, laparotomy with resection is recommended in adults with intussusception due to an increased association with malignancy or other benign pathologies [1, 2, 8–10].
Rectal prolapse associated with intussusception is rarely reported in the literature. Preoperative diagnosis can be difficult and may lead to a delay in diagnosis [1, 7, 10–12]. There are even fewer reports of carcinoma as a lead point of intussusception with associated prolapse through the anus [4, 8, 13–15]. We contribute to the existing literature by presenting another rare case of rectal carcinoma leading to intussusception with rectal prolapse.
CONCLUSION
Rectal prolapse associated with intussusception is a rare condition not frequently reported in the literature. In adults, carcinoma is often the lead-point of the intussusception. We present a rare combination of rectal prolapse, intussusception and malignancy. Difficulty in diagnosis and delayed intervention are associated with poor prognosis. Surgical intervention is imperative to limit the complications.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
Data sharing is not applicable to this article as no new data were created or analyzed in this study.



