-
PDF
- Split View
-
Views
-
Cite
Cite
Alhasan H Alhebshi, Mohammed Aldekhail, Alaa Abduljabbar, Perianal extramammary Paget’s disease with adenocarcinoma of perianal skin area, a case report, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad291, https://doi.org/10.1093/jscr/rjad291
Close - Share Icon Share
Abstract
Extramammary Paget disease (EMPD) is an uncommon slow-growing skin adenocarcinoma originating in the anogenital region and axilla outside the mammary glands, often in regions with apocrine glands. The most common location is the vulva, followed by perineal, perianal, scrotal and penile skin. Here, we report a case of a 63-year-old male with EMPD in the perianal region. He reported 4 years of pain associated with an increasing region of skin irritation and bleeding on defecation that did not improve with topical agents. A biopsy sample revealed poorly differentiated carcinoma consistent with adenocarcinoma and associated with Paget disease. Workup was done. The patient tolerated local excision of the region well with no complications. A rare disease, EMPT, is challenging to diagnose and manage. Histopathological findings can, however, differentiate it from a wide array of similar skin conditions. Thorough investigations should be undertaken before initiating treatment to ensure the best outcomes.
INTRODUCTION
Paget disease was first described and named by Sir James Paget, who in 1874 described a skin lesion around the nipple that looked similar to eczema and had underlying breast malignancy potential [1]. Extramammary Paget disease (EMPD) is an uncommon and slow-growing skin adenocarcinoma that originates in the anogenital region and axilla outside the mammary glands [2], often in regions with apocrine glands [3]. The most common location for EMPD is the vulva, followed by perineal, perianal, scrotal and penile skin [4].
EMPD is typically characterized as an erythematous, nonspecific, eroded scaly plaque with ulcerations and pruritic lesions [5]. This condition is classified as primary or secondary. The primary form originates from the epidermis or adnexal structures, whereas the secondary form originates in association with another source of internal malignancy such as the urinary or gastrointestinal system [6].
Diagnosis of this disease is extremely challenging, requiring histopathological analysis as the gold standard for confirmation. Such analysis shows Paget cells containing cytoplasm that is clear and pale, as well as circles of hypochromatic large nuclei and clusters [7]. Diagnostic challenges include the similarity of EMPD to common skin conditions such as psoriasis, eczema and dermatitis [8].
As this condition may or may not be associated with malignancy, a thorough investigation ensures no metastasis by means of the lymphatic system or other adjacent structures such as the rectum and urinary system [9]. Because of the rare occurrence and unclear pathogenesis of EMPD, no standardized treatment guidelines have been published. Nonetheless, local wide excision is considered standard therapy [10]. Some patients may not be suitable candidates for surgery because of comorbidities and surgical risks, which include but are not limited to anesthesia risks, functional decline and surgery-related complications. Other treatment methods have also been suggested, such as radiotherapy, which is less invasive and has curative potential [11].
CASE REPORT
A 63-year-old male who was hypertensive and had not undergone prior surgery was referred to us from a local hospital after reporting 4 years of perianal pain associated with skin irritation and bleeding on defecation (Fig. 1). Two years after the pain began, he noticed increasing perianal swelling that did not improve with the use of topical agents. He denied any significant weight loss or family history of such a skin condition. The local hospital investigated the perianal mass and swelling by performing a biopsy, the sample showing a poorly differentiated carcinoma consistent with adenocarcinoma that was associated with Paget disease. A computed tomography (CT) scan of the abdomen and pelvis showed anal canal thickening with no lymphadenopathy.

On examination of the patient at our hospital, rectal inspection showed a well-defined erythematous plaque extending from the anus, its right lateral side showing a verrucous surface extending 14 cm from the scrotum to the coccyx and 30 cm laterally. A 4 × 4 cm mass that was soft but not tender and bled easily was located at the anal verge in the anterolateral aspect to the left side. In addition, there were two small masses on the right side, 5 cm from the anus.
The case was discussed in a multidisciplinary team meeting after multiple radiological and laboratory investigations were performed to exclude other tumors or metastasis. A repeated CT scan showed no evidence of metastasis, with a borderline bilateral inguinal lymph node. A magnetic resonance imaging scan showed a perianal mass not extending into the anal canal with mild proximal sigmoid colon wall thickening. A positron emission tomography (PET) scan showed focal intense fluorodeoxyglucose (FDG) uptake in the region below the anal verge, focal moderate FDG uptake noted in the sigmoid colon and mild FDG uptake in the bilateral mildly enlarged inguinal nodes not consistent with metastasis, with no other evidence of metastasis. It was decided to proceed with a colonoscopy and fine needle aspiration (FNA) of the groin lymph node.
A colonoscopy was performed to the terminal ileum with no pathological findings, and FNA of the left inguinal lymph node was negative for metastasis. The patient also underwent perianal swelling excision, with histopathological findings confirming a poorly differentiated adenocarcinoma. We discussed the possibility of chemoradiation with him, but he refused. He was lost to follow-up but returned with the same concern, and it was decided to do a punch biopsy in all quadrants around the anal region to assess for recurrence. All quadrants showed EMPD except at the 10 o’clock position, which showed a poorly differentiated adenocarcinoma and EMPD. The patient underwent local excision of that region (Figs 2 and 3) and a further FNA inguinal lymph node biopsy was planned if the pathological results were positive with positive margins.

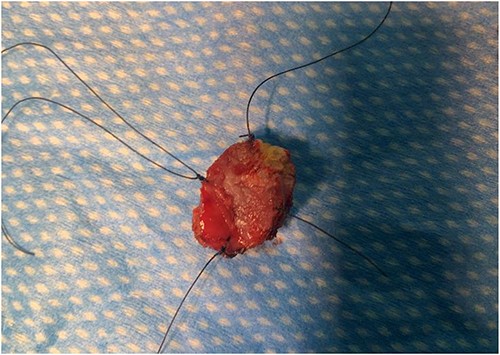
The surgical pathology results revealed a poorly differentiated adenocarcinoma with EMPD, as well as a positive lateral and deep margin for adenocarcinoma. FNA was also performed for the right inguinal lymph node biopsy, which showed metastatic adenocarcinoma. We are currently offering the patient a stoma creation and removal of the entire skin lesion, to be further discussed in the multidisciplinary team meeting. The patient was followed by the oncology department and advised to undergo chemotherapy, but he refused treatment. He is currently being followed by colorectal services (Fig. 4).

DISCUSSION
EMPD is an exceptionally rare disease that is considered an intraepidermal carcinoma that develops in areas of the body rich in apocrine glands. However, when cancer cells spread beyond the basement membranes, reach the dermis and form a nodule, this disease develops into invasive forms of skin cancer in general [12].
Clinical characteristics of this disease were reported in a study that showed that erythema was a common clinical characteristic for all lesions. Nodules were present in around 24% of cases, an erosion in 49% and hypopigmentation in 25%. In addition, lymphadenopathy was present in around 39% of cases [13]. This disease has diverse symptoms and poor prognosis in terms of expansion, deep invasion and distant metastasis [5]. The estimated median time delay before correct diagnosis of EMPD is 2 years [14].
EMPD has been associated with underlying disease in around 12–33% of cases. For this reason, patients should be investigated thoroughly after diagnosis for an occult primary malignancy [15], including colon, bladder and breast cancer, by means of colonoscopy, cystoscopy and imaging [15]. Our patient underwent thorough investigations by colonoscopy, CT scan and PET scan, as well as biopsies of the lesion and lymph nodes, to ensure that there was no metastasis.
Multiple factors have been associated with recurrence. Patients with positive lymph node disease have a 33% chance of developing a distant metastasis. Other contributing factors for recurrence and hence a poorer survival rate include the thickness of the tumor, the status of lymphovascular invasion, the number of lymph node metastases and older age [16].
Surgical excision is the main therapeutic modality used to treat this condition [11]. Topical management with imiquimod 5% has been tried, with 52.4% of patients showing a complete response and 28.6% a partial response after a mean duration of treatment of 16 weeks [15]. We used both modalities for our patient, first topical management, which according to the patient provided only a partial response but did not resolve the issue, and then surgical intervention.
Multidisciplinary meetings are advisable for such a rare disease when evidence and guidelines for its management are lacking in order to discuss various suitable treatment modalities, such as chemotherapy and radiotherapy along with surgical intervention and topical management [3]. In our case, a multidisciplinary team was involved from the beginning and their recommendations have been followed to ensure best outcomes.
CONCLUSION
EMPD is a rare disease with diverse symptoms that mimic those of other common dermatological conditions. This presents a challenge in diagnosing the disease and leads to delayed presentation and poor prognosis. EMPD has the potential for metastasis; hence, thorough investigations should be undertaken to exclude other primary cancers. Surgical intervention remains the mainstream treatment modality.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest to declare.
FUNDING
None.
CONSENT AND ETHICAL APPROVAL
The patient provided verbal consent in the clinic and over the phone. Ethical approval was granted by King Faisal Specialist Hospital and Research Center in Riyadh (approval number: 2225404).



