-
PDF
- Split View
-
Views
-
Cite
Cite
Mahmoud Najm, Aya Kelzia, Ibrahim Arnaout, Lama Kadoura, Ahmad Ghazal, A rare case of small bowel obstruction caused by Meckel’s diverticulum: case report, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad332, https://doi.org/10.1093/jscr/rjad332
Close - Share Icon Share
Abstract
Meckel’s diverticulum MD is the most common congenital deformity of the gastrointestinal tract. It has a very low reported incidence. We reported a 9-year-old child complaining of symptoms of small bowel obstruction. He had no medical or surgical history. There is no signs of peritonitis and appendicitis. Simple abdominal X-ray diagnosed the obstruction, during surgery we found an MD located 30 cm from the ileocecal valve, fibrous band may be as complication for MD to the anterior abdominal wall at the umbilicus, the small intestines were wrapped around the band, causing the obstruction. The MD and the band were excised with end-to-end anastomosis. We diagnosed our case during surgery. Early surgery is important to preserve bowel from gangrene or necrosis. The patient’s well-being improved, and he was discharged from the hospital in good condition.
INTRODUCTION
Meckel’s diverticulum (MD) is the most common congenital deformity of the digestive tract that occurs in 2% of the population [1, 2]. This diverticulum occurs because of incomplete obliteration of the vitelline or omphalomesenteric duct, which occurs in the 5th–7th week of fetal growth [3].
It is generally asymptomatic, and only 2% of cases are symptomatic [2]. In children, gastrointestinal bleeding and intestinal obstruction are more common [4]. Obstruction may occur because of torsion of the diverticulum. We report a case that presenting with small bowel obstruction because of wrapping of the small intestine around a fibrous band from MD to the umbilicus [5].
CASE PRESENTATION
A 9-year-old child presented at the emergency department at our hospital after 4 days with symptoms of small bowel obstruction, including diffuse abdominal pain, nausea, vomiting, constipation and abdominal distension. His past medical history was not significant, and he had no surgical history. The abdomen was breathing, smooth, tender without rebound tenderness; no signs of peritonitis and appendicitis were appreciated. His rectal examination was unremarkable. A pulse rate of 100/min. The abdominal X-ray showed multiple air-fluid levels (Fig. 1). A diagnosis of small bowel obstruction was made; the patient underwent intravenous fluid therapy and nasogastric tube insertion before undergoing surgical intervention that involved midline incision and exploratory laparotomy. During surgery, the small intestine was found to be dilated and congested, with an MD located 30 cm from the ileocecal valve, associated with a fibrous band connected to the anterior abdominal wall at the umbilicus. The small intestines were wrapped around the fibrous band, causing the obstruction (Figs 2 and 3). The intestines were released, the MD and the band were excised with end-to-end anastomosis and a pelvic drain was inserted. The patient was discharged. By follow-up, the patient showed no evidence of complications.

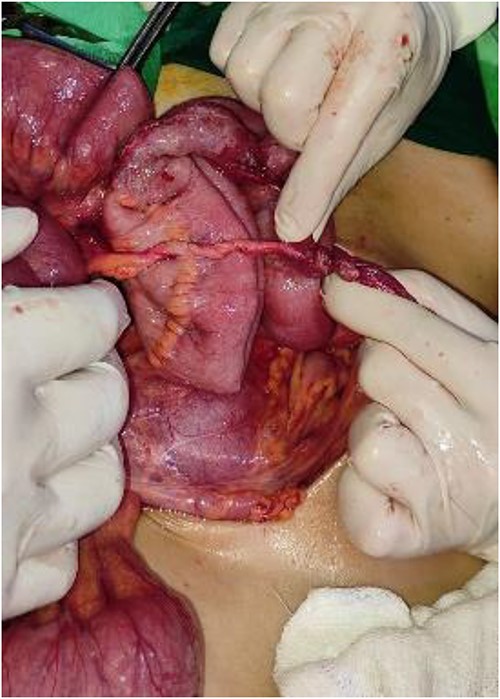
The fibrous band connected to the umbilicus, where the small intestines were wrapped around the band.

DISCUSSION
MD is the most common congenital malformation in the lower portion of the small intestine [1, 2]. The cause of this diverticulum is the vitelline duct, which normally connects undeveloped gut to the yolk sac that will atrophies during 5th–7th week of pregnancy [3]. When the vitelline duct did not atrophy completely then it develops into a true diverticulum, which makes up 2% of population [2]. Most people with diverticulum are asymptomatic [2]. Symptoms appear usually during the 1st year of life, with the possibility of their appearance during childhood [2]. These symptoms include rectal bleeding or intestinal obstruction [4]. Our case presented with small intestinal obstruction and we confirmed it through abdominal X-ray. The intervention was surgical that involved midline incision. During the surgery, it was revealed that there was the MD, located 30 cm from ileocecal valve and bloody supplied by yolk arteries [2, 4]. Intussusception or inversion of the MD into the ileum or cecum, or the existence of the fibrous band that entraps the vascular supply of the small bowel underneath it and may lead to strangulation, or wrap the small intestines around the fibrous band from MD to the umbilicus [4].That happens commonly for people who have diverticulum with obstruction symptoms [4]. The fibrous band is a remnant of right and left yolk arteries [4]. The anatomical structure for the diverticulum of length and base is important factor for rotation around the band thus occurrence of obstruction [6]. In other cases, reported pre-operate diagnosis is rare by 4% of their cases. MD can be diagnose by ultrasound when there are complications and it is not specific [7]. Arteriography and technetium pertechnetate scanning are good for diagnosis in case with bleeding or ectopic gastric mucosa [8].
Finally, laparoscopy for diagnosis is also useful in case with complications [1, 2]. We diagnose our case when we made surgical intervention. The treatment of MD can be done by laparoscopy or open surgery. Symptomatic diverticulectomy is safe with the rate of morbidity 2% and mortality 1% [9]. In our case, we use open surgery, and the diverticulum and the band were removed with end-to-end anastomosis. Then a histological examination of the diverticulum was performed, which was with normal results. This case may have manifestations similar to those of acute appendicitis, inflammatory bowel disease or other causes of small bowel obstruction [4].
CONCLUSION
Fibrous band may be a complication for MD, which may make a part of the small intestine to wrap around it and then symptoms of bowel obstruction appear. Early surgery intervention, diverticulectomy, band resection and bowel release are very important, as in our case.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No sources of funding.
DATA AVAILABILITY
All data is available in the article.
CONSENT
The authors obtained written informed consent from the patient’s father for this publication.
GUARANTOR
Mahmoud Najm is the guarantor of this article.



