-
PDF
- Split View
-
Views
-
Cite
Cite
Carolina Baz, Gioia Pozza, Marco Di Pangrazio, Francesco Toti, Nicolas H Dreifuss, Antonio Cubisino, Gabriela Aguiluz, Alberto Mangano, Jesús Rondón, Pier Cristoforo Giulianotti, Robotic surgery: extending the minimally invasive approach in patients with splenomegaly. A case report, Journal of Surgical Case Reports, Volume 2023, Issue 6, June 2023, rjad325, https://doi.org/10.1093/jscr/rjad325
Close - Share Icon Share
Abstract
Splenomegaly represents a challenge during splenectomy. Despite the laparoscopic approach becoming the gold standard for spleen removal, it remains controversial in this condition since the limited working space and increased risk of bleeding portray the leading causes of conversion, preventing patients from experiencing the benefits of minimally invasive surgery. The robotic platform was used to perform a splenectomy on a 55-year-old female with severe thrombocytopenia due to a relapsed large B cell lymphoma with splenomegaly. The advantages of this approach, favoring less blood loss and precise movements in a small surgical field, may allow MIS to become the first choice in this unfavorable setting, even in hematologic malignancies, which are associated with higher complication rates.
INTRODUCTION
Splenomegaly, for most authors, is considered when the spleen weight exceeds 1000 g or the length of 20 cm [1]. While undergoing surgery, this condition is associated with greater challenges, such as spleen retrieval, hemorrhage, given the difficulty in controlling inflow and outflow, and avoiding injury of the tail of the pancreas, exposing patients to a higher rate of complications when compared to normal-sized ones. Among them, intraoperative bleeding is the most feared one, increasing the conversion rates [1–3]. Since the first laparoscopic splenectomy was reported by Cuschieri et al. [4], given the well-known benefits of minimally invasive procedures [3, 5], laparoscopic surgery has become the preferred approach for spleen removal [1, 6]. However, despite some authors acknowledging its feasibility in cases of splenomegaly [1, 7], others have published their concerns regarding the utilization of laparoscopy [8, 9]. Combined treatment with preoperative splenic artery embolization has proven to reduce intraoperative blood loss and conversion rate while improving the hematological parameters [1, 2, 10]. Nevertheless, the technical challenges of laparoscopy in this scenario remain. The robotic platform, with its wider range of motion and improved ergonomics, among other features [11, 12], can overcome these difficulties, thus allowing patients to experience the benefits of minimally invasive surgery (MIS).
CASE REPORT
The patient was a 55-year-old female with relapsed large B cell lymphoma, severe thrombocytopenia with 17,000 platelets, and splenomegaly. Computed tomography (CT) (Fig. 1) and magnetic resonance (MR) (Fig. 2) images showed an enlarged spleen with multiple lesions, the largest measuring 3.5 cm, suspicious for lymphoma. Given the increased risk of intraoperative bleeding during splenectomy, a splenic artery embolization was performed the day before by using an Amplatzer plug (Fig. 3A and B), and platelets and fresh frozen plasma were prepared for the operation.
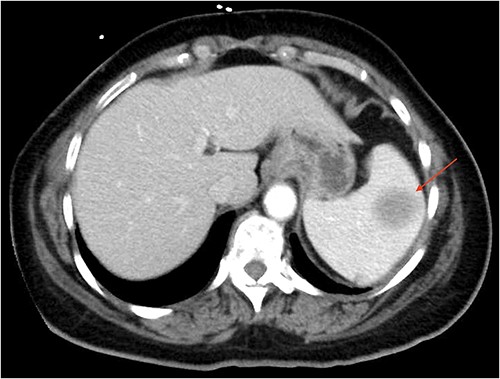
CT of the abdomen (axial section) showing an enlarged spleen with a 3.5 cm lesion.

MR imaging of the abdomen (coronal section) revealing an enlarged spleen with multiple lesions, the largest one with heterogeneous enhancement.
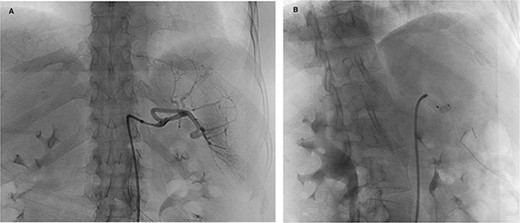
Preoperative splenic artery embolization (A: angiogram, B: post-plug deployment).
A robotic splenectomy was carried out. The spleen was enlarged and highly perfused (Fig. 4). After opening the gastrocolic ligament, the splenic artery was visualized. The short gastric vessels were divided with the vessel sealer using a double coagulation technique to decrease the chances of re-bleeding. Once the left gastroepiploic artery was sectioned, the left colonic flexure and the lower pole of the spleen were mobilized. The tail of the pancreas was exposed, and a vessel loop passed behind the main splenic pedicle, which was divided with a vascular stapler (Fig 5A and B). The ligament of the spleen was dissected using the monopolar hook. Posteriorly, an anomalous vein branch draining from the splenic circulation into the left renal vein (spontaneous splenorenal shunt) was seen, dissected and divided between clips (Fig. 6A and B), and a total ‘en-block’ splenectomy with the lymphonodi at the hilum was performed. Proper hemostasis was confirmed; blood loss was minimal, being <50 cc. The operative time was 122 minutes. The patient was discharged on post-operative day 2 with a platelet count of 204,000.
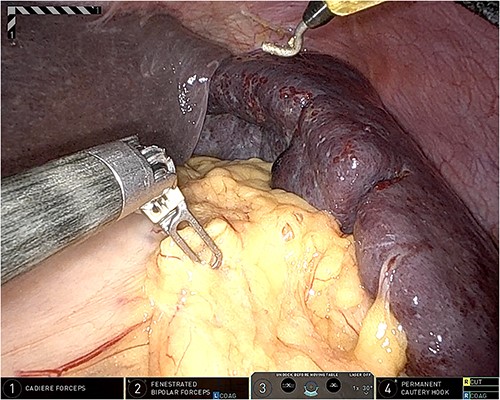
Intraoperative picture showing an enlarged and highly perfused spleen.
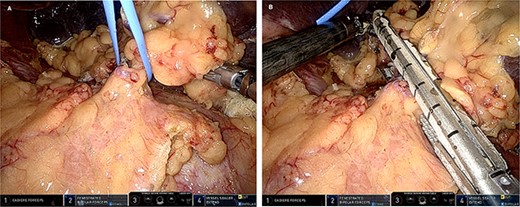
(A) Intraoperative picture displaying the splenic main pedicle surrounded by a vessel loop; (B) intraoperative picture unveiling the division of the splenic main pedicle using a vascular stapler.
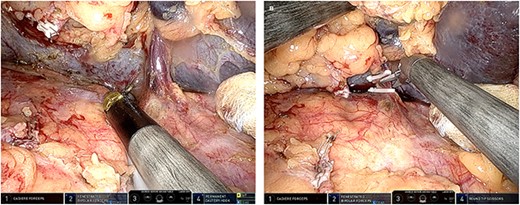
(A) Intraoperative picture exhibiting the dissection of a spontaneous splenorenal shunt; (B) intraoperative picture exhibiting the division of the spontaneous splenorenal shunt division between clips.
DISCUSSION
Splenectomy has been performed since the 1950s for hypersplenism, but despite ending with induced cell blood destruction, morbidity due to severe complications was reported to reach up to 26.6% with open surgery [3, 13]. For this reason, MIS has been widely adopted due to its proven benefits, including less blood loss and post-operative pain, a shorter hospital stay and better cosmesis [3, 5]. Several publications have shown the advantages of this approach for spleen removal, thus allowing laparoscopy to be accepted as the ‘gold standard’ for splenectomy. Rosen et al. [14] retrospectively reviewed a consecutive series of laparoscopic splenectomies performed for nontraumatic, splenic pathology at the Cleveland Clinic Foundation, outlining shorter operations, minimal blood loss and earlier discharge for benign indications. In their meta-analysis, Winslow et al. [3] compared the complications between laparoscopic and open splenectomy, reporting a significant reduction in splenectomy-related morbidity (15.5 vs. 26.6%) mainly associated with fewer pulmonary, wound and infectious complications. However, laparoscopy’s benefits are unclear for patients with splenomegaly. Although some authors have supported its viability [1, 7], the limited working space and the difficulty in controlling bleeding have been recognized to increase the operative time, conversion rate and post-operative morbidity [8, 9]. Moreover, during the laborious dissection, capsule breakage could lead to splenosis [6]. According to Reso et al. [1], most conversions to open splenectomy are due to intraoperative bleeding, ranging from 6.6 to 18%, with portal hypertension increasing the risk for hemorrhagic complications [2]. In hematologic malignancies, laparoscopic splenectomy has even higher conversion rates and blood loss when compared with benign diseases [14]. Patients tend to have larger spleens, which implies increased technical difficulties for hilar control, splenic mobilization and maintenance of oncologic principles. For all these reasons, splenomegaly has even been considered to be a contraindication to the laparoscopic approach in some centers [8]. Preoperative splenic artery embolization has been utilized to decrease the associated complications. Reports have demonstrated not only reduction of blood loss and conversion rate [1, 2, 10] but also the increase of the platelet count 2–4 hours after embolization completion [15]. Nevertheless, laparoscopy in this scenario remains challenging due to its limitations regarding the lack of articulated instruments and the 2D visualization of the surgical field [12], which can prevent patients with splenomegaly from experiencing the benefits of the minimally invasive approach. The robotic platform, designed to overcome the restrictions of laparoscopy, incorporated a wristed range of motion, a magnified 3D view of the operative field and optimized ergonomics [11, 12]. Nota et al. [12] stated that the technical advantages given by the robotic approach reduce blood loss and grant for the utilization of MIS in areas difficult to reach using laparoscopy, which could extend the indications for MIS in oncological procedures. By allowing to work comfortably in a reduced surgical field and improving precision and visualization, these features may also address the main drawbacks of laparoscopy for splenomegaly.
Despite robotic surgery experiencing constant growth, still, scarce data have been published regarding its specific use for splenectomy in the case of splenomegaly. Even though further experience is needed to assess the impact of this approach on patient outcomes, its established benefits in other procedures may pave the way to favor robotic surgery to become the new ‘gold standard’ for splenectomy in patients with splenomegaly, even in the case of hematologic malignancies, associated to the highest complication rates with the use of laparoscopy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research received no specific grant from funding agencies in the public, commercial or not-for-profit sectors.
DATA AVAILABILITY
No new data were generated or analysed in support of this research.



