-
PDF
- Split View
-
Views
-
Cite
Cite
Anže Lamut, Simon Kovač, Complications of surgical management of osteopetrosis. A case report of multiple surgeries performed on one patient, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad315, https://doi.org/10.1093/jscr/rjad315
Close - Share Icon Share
Abstract
Osteopetrosis is a rare form of sclerosing bone dysplasias which in some cases requires orthopedic surgical management of its complications. It is characterized by osteosclerosis, brittle bones and obliteration of the medullary cavity. Therefore, surgery in these cases is difficult and results can be compromised by postoperative complications. We present a case of a 73-year-old patient treated at our institution in a period of 24 years. In this period, the patient had bilateral primary hip arthroplasty (THA), total knee arthroplasty, revision surgeries of both THA’s and lumbar spine surgeries. The treatment of infected THA and periprosthetic fractures ended with satisfactory results but complications of the spinal surgery resulted in a poor clinical outcome.
INTRODUCTION
Osteopetrosis is a rare congenital bone disorder of sclerosing bone dysplasias. It is characterized by osteosclerosis, brittle bones and obliteration of the medullary cavity due to reduced osteoclastic bone resorption [1, 2].
There are three types of the disease: infantile malignant (autosomal recessive), intermediate (autosomal recessive) and benign (autosomal dominant, ADO). The ADO form is the most common and from an orthopedic perspective, the most important [1]. It clinically manifests with frequent fractures, osteoarthritis, coxa vara, long-bone bowing, osteomyelitis and fracture non-union [1].
The diagnosis of ADO is based on clinical and radiographic findings. Radiographic imaging of the pelvis, long bones, phalanges and vertebrae often shows a ‘bone within bone’ or ‘endobones’ appearance and ‘rugger jersey spine’ on the axial skeleton radiographs [3, 4].
Surgical treatment of the patients with osteopetrosis is challenging. Orthopedic manifestations are best treated conservatively and symptomatically [4]. The brittleness of the bone, osteosclerosis and obliteration of the medullary canal make surgery difficult. During drilling, reaming and sawing, drill bits and other tools can overheat and break. Most common postoperative complications are osteomyelitis, periprosthetic fractures and fracture non-union [5].
The present case report presents a patient with ADO treated with several different surgeries, the majority of which were performed at our facility.
CASE REPORT
A 73-year-old man showed himself to our hospital in 1989, complaining of left hip pain. X-ray imaging revealed advanced osteoarthritis of the left hip as well as skeletal abnormalities pathognomonic for osteopetrosis. Following earlier intertrochanteric osteotomies carried out elsewhere, there was osteosynthetic material present in the right femur. A cementless isoelastic total hip arthroplasty (THA) was performed (Fig. 1). The greater trochanter was fractured and repaired with screws and cerclages.

Isoelastic uncemented hip arthroplasty. Broken trochanteric part was fixed with cerclage wires and screws.
In 2008, the patient complained about increasing pain in the left hip. Laboratory tests were normal and X-ray imaging showed a loose cup which was replaced with a reinforcement ring and a cemented cup and the loose femoral component which was exchanged with a cementless revision stem (Fig. 2). Routine intraoperative tissue samples were positive and Staphylococcus epidermidis was isolated. A 3-month antibiotic treatment consisted of ciprofloxacin and rifampicin successfully cured the infection.

Anteroposterior radiograph of the left hip after revision surgery in 2008.
In 2011, a cementless THA of the right hip was done for the osteoarthritis. Three residual broken screws were present in the distal diaphysis from previous surgeries and were left in place (Fig. 3).
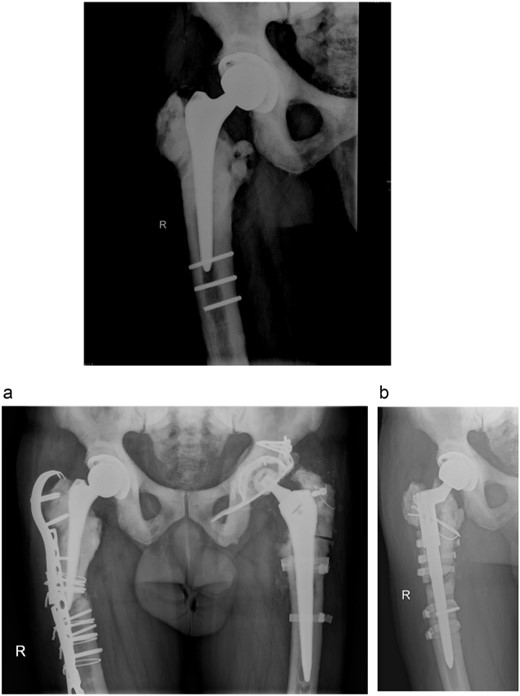
Anteroposterior radiograph of the right hip after THA with three broken residual screws in the distal diaphysis. (a) Anteroposterior hip radiograph with broken lateral plate. (b) Anteroposterior radiograph of the right hip after exchanging the femoral stem.
In 2012, the patient presented with a stress fracture of the right tibial diaphysis. It was treated with osteosynthesis with plate and screws after a 4-month conservative treatment with plaster of Paris. It healed uneventfully.
In 2013, the patient suffered a spontaneous Vancouver B2 periprosthetic fracture of the right THA. Osteosynthesis with a locking plate with screws and cerclages was done. Three months after the surgery, the plate broke and was exchanged with addition of an anterior plate and autologous spongioplasty. However, osteosynthesis failed 8 months later and the firmly ingrown femoral component was revised (Fig. 3a). Proximal femoral osteotomy resulted in several broken fragments. During removal of the broken screws, three sets of removal instruments were destroyed. A cementless revision modular stem was inserted and bone fragments fixed with cerclage wires and titanium tapes (Fig. 3b). Surgery took 6 h and he received six units of blood. Microbiological tissue samples were negative.
In 2015, he underwent an elective cemented right total knee arthroplasty. To avoid the opening of the femoral canal, patient specific jigs were used.
Six months later, he complained about lumbar pain which irradiated into the right thigh and knee. A CT scan of the lumbar spine showed multiple lumbar spine stress fractures, and CT myelography showed complete obstruction at L2–3 level (Figs 4 and 5). Conservative therapy was ineffective. Therefore, the patient was transferred to a spinal center. There he underwent L2–L3 decompression with short-term effect because decompression resulted in instability. 360° spondylodesis was done; however, it resulted in non-union, and the material was removed (Fig. 6).


Sagittal view of CT lumbar spine myelography. Note also the density of sclerotic bone.

Lateral radiograph of the lumbar spine after failed 360° spondylodesis.
In 2019, he presented himself due to high fever and pain in the abdomen and left thigh after recovering from cystitis. A periprosthetic infection of the left THA and septic arthritis of the left knee were diagnosed. Debridement of the THA and replacement of the prosthetic head was performed, as well as arthroscopic lavage of the knee. Postoperatively, a combination antibiotic therapy was initiated due to multiple bacterial strains isolated. After the period of acute antibiotic therapy, life-long suppression antibiotic therapy consisting of minocycline was initiated.
Due to excruciating back pain, the patient is at the moment wheelchair-ridden and mobile only on short distances with crutches, and without signs and symptoms of infection.
DISCUSSION
The optimal surgical strategy of osteopetrosis-related disorders has not been clearly determined. Although cemented total knee arthroplasty is the standard operative treatment of knee osteoarthritis, hip arthroplasty can be cemented or cementless. Cemented stems can be used to avoid intraoperative fractures. However, poor adhesion between cement and the bone is a concern [6].
There are only two reports on lumbar spinal fusion in osteopetrosis. In both cases, spondylodesis healed. Both cases proved technically demanding due to hard and brittle bone [7, 8].
To the best of our knowledge, the current report presents the patient with the largest number of different orthopedic procedures. The patient had several complications which include low-grade periprosthetic infection, acute hematogenous periprosthetic infection, non-union of a periprosthetic fracture and failure of spondylodesis. Nevertheless, from the first THA, he had 20 years of quality life. This is, to our knowledge, also the longest follow-up time of THA in a patient with osteopetrosis.
Treatment of periprosthetic infections in patients with osteopetrosis has not been reported. In our case, we followed our standard treatment protocol for low- and high-grade periprosthetic infection. Treatment was successful in both cases; however, due to sub optimal surgical treatment of high-grade infection of the left THA, we decided to implement chronic antibiotic suppression with minocycline.
In conclusion, we have reported a unique case of surgical treatment of patient with ADO. We successfully managed various periprosthetic complications, but postoperative spinal complications resulted in an overall poor clinical outcome.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
All data found about this case are included in this published article.



