-
PDF
- Split View
-
Views
-
Cite
Cite
Abbas Karimi, Samira Derakhshan, Pouyan Aminishakib, Hiva Saffar, Kimia Hafezi Motlagh, Central oral pulse granuloma: a case report of huge mandibular jaw lesion, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad312, https://doi.org/10.1093/jscr/rjad312
Close - Share Icon Share
Abstract
Oral pulse granuloma is a rare lesion of the oral cavity with unclear etiology. Some authors believe this lesion is a foreign body reaction to implanted food particles. In the oral cavity, most cases are found in the posterior regions of the mandible. The edentulous mandible was involved in 20 cases with oral pulse granuloma. In these cases, the premolar–molar site was the most common region. Here we present a case of a 70-year-old male with huge unilateral swelling of the mandible on the left side. This paper aims to present a case of oral pulse granuloma with wide extension, detailed clinicohistopathologic features with 2-year follow-up and a short review of reported cases.
INTRODUCTION
Oral pulse granuloma is a rare lesion of the oral cavity that was first introduced by Lewars [1] as an inflammatory lesion in the buccal sulcus of a patient wearing a mandibular denture. Various names, such as chronic mandibular periostitis, hyaline body granuloma, oral vegetable granuloma and giant cell angiopathy, have been suggested for this lesion, and finally, oral pulse granuloma was chosen [2]. These lesions in the oral cavity are often seen in the edentulous jaw or in patients with a history of dental treatments. There are reports of their presence in the wall of the periapical/residual cyst, dentigerous cyst and ameloblastoma. The age range is 6–70 years, and mandibular involvement has often been reported in the molar–premolar area [3]. Symptoms of the lesion include pain, swelling and discharge. The radiographic view of oral pulse granuloma is not pathognomonic. Intraosseous types are seen as irregular radiolucency with remnants of bony trabeculae that can mimic the appearance of many jaw lesions and extracellular types with poorly defined erosion appearance [2]. Chou et al. divided oral pulse granuloma into central and peripheral groups based on their location. Central oral pulse granulomas are usually asymptomatic lesions and peripheral lesions are seen as submucosal swelling [4]. There is no consensus on the etiology of oral pulse granuloma. Some authors believe that the hyaline rings in this lesion are the remains of foreign bodies and vegetables, especially beans and peas. But some other researchers believe that hyaline rings are a sign of the presence of blood vessels or degenerated collagen fibers. Some have linked these lesions to infection with Torulopsis glabrata [5].
In this report, we present an example of oral pulse granuloma with a 2.5-year follow-up, which is unique in terms of lesion size and extent of involvement, as well as radiographic appearance.
CASE PRESENTATION
The patient was a 70-year-old man with a complaint of unilateral swelling of the face on the left side of the mandible, which occurred 4 months ago. He referred to the Faculty of Dentistry, Tehran University of Medical Sciences. On intraoral examination (Fig. 1), hard bony swelling was observed extending from the first premolar to the posterior mandible with obliteration of the vestibule. The mucosa covering this swelling was the normal mucosa of the mouth. The patient did not report a history of significant systemic disease. In the orthopantomograph image, irregular multilocular radiolucency was observed, with distinct septa from the anterior mandible extending distally to the ramus (Fig. 2). Perforation of the lower mandibular cortex was also visible in some areas. Computed tomography (CT) showed a Hypodense osteolytic lesion on the left side of the mandible, extending from the anterior region to the molar region. CT image also showed buccolingual expansion and cortical perforation on the buccal and lingual side, indicating a locally aggressive lesion.
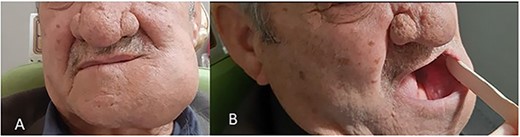
Preoperative views of the lesion. (A) Extraoral evaluation of the lesion showed huge mandibular swelling on the same side with intact skin. (B) Intraoral evaluation of the lesion showed left mandibular swelling with intact mucosa.

Panoramic view showing irregular multilocular radiolucency from the anterior mandible extending distally to the ramus.
An incisional biopsy was done, and a histopathological examination revealed the myxoid tissue with inflammatory infiltration. The patient was subjected to surgical excision by a maxillofacial surgeon.
After the complete excision of the lesion (Fig. 3) and reconstruction of the mandible and ramus by the plate, the sample was sent for histopathologic evaluation.
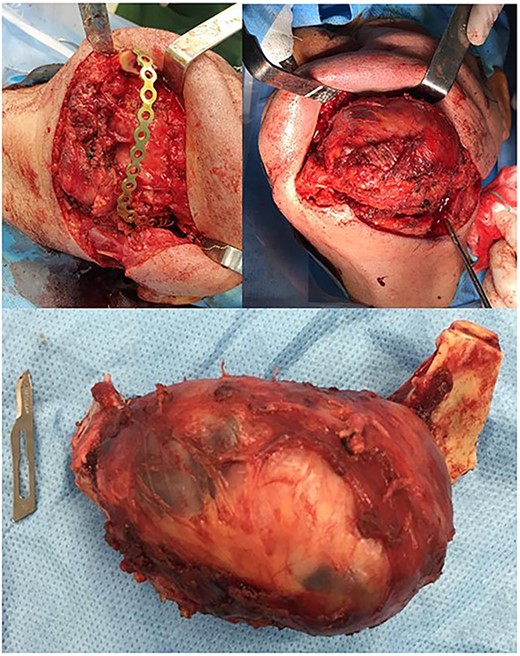
Complete surgical excision of the lesion and reconstruction of the mandible and ramus.
Microscopic examination showed (Figs 4–7) inflamed connective tissue composed of prominent plasma cells mixed with numerous osteoclastic multinucleated giant cells of various sizes with intracytoplasmic asteroid bodies and round Schaumann bodies, which surrounding round to amorphous eosinophilic areas composed of the spindle to stellate cells in fibromyxoid background is also evident.
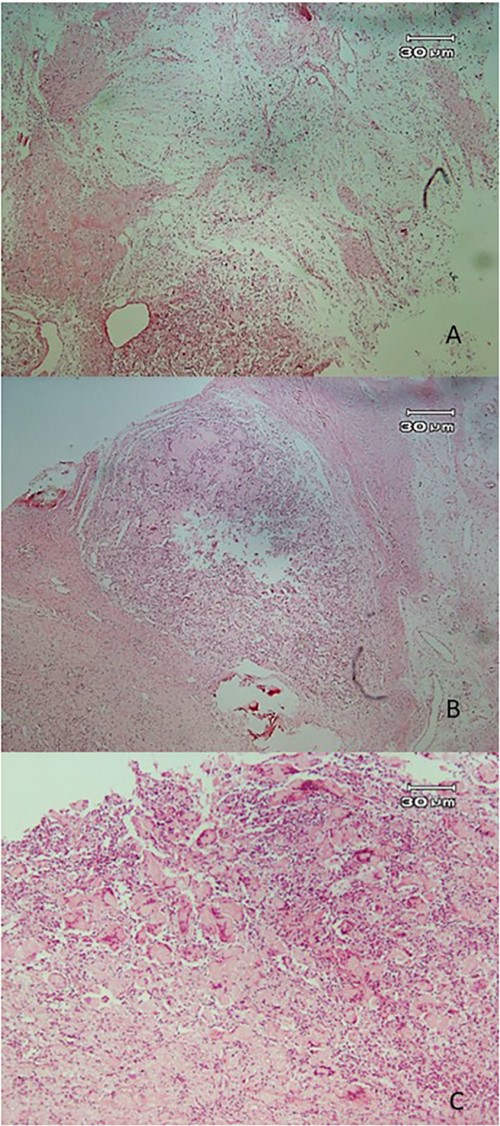
Histopathologic views of the lesion (H&E staining, ×100 magnification). (A) Inflamed fibromyxoid connective tissue. (B) Area of one granulomatous pattern inflammation with multiple giant cells. (C) Numerous foreign body giant cells admixed with severe chronic.
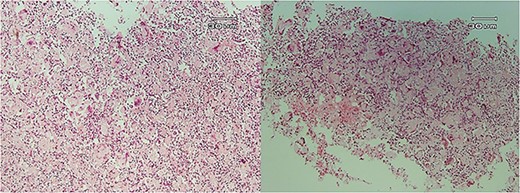
Histopathologic views of the lesion (H&E staining, ×10 magnification). Inflammation in the connective tissue and foreign body giant cells admixed with severe chronic inflammatory cells.
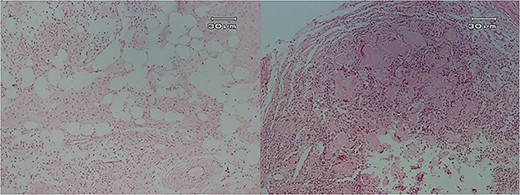
Histopathologic views of the lesion (H&E staining, ×100 magnification). Inflamed fibromyxoid connective tissue and foreign body giant cells.
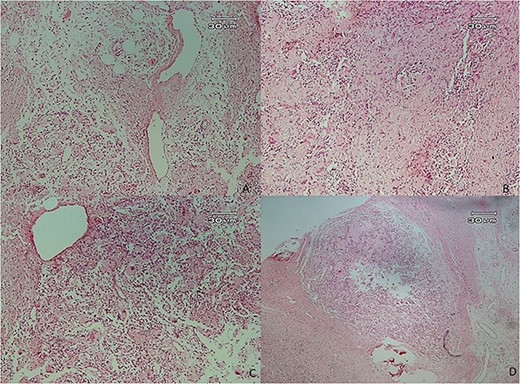
Histopathologic views of the lesion (H&E staining×100 magnification) showing chronic inflammatory cells admixed with multinucleated giant cells of varying sizes.
Immunohistochemical evaluation was done to identify the cell types involved in the inflammatory response or the incidence of degeneration in muscular fibers and showed SMA and desmin positive in vessel walls, S100 negative and CD56 positive in giant cells and macrophages, confirming the foreign body reaction mediated by macrophages. Congo red staining was also negative. A diagnosis of inflamed fibrotic connective tissue with prominent giant cell-rich foreign body reaction incompatible with oral pulse granuloma was made.
No evidence of recurrence was observed after 2 years (Fig. 8).
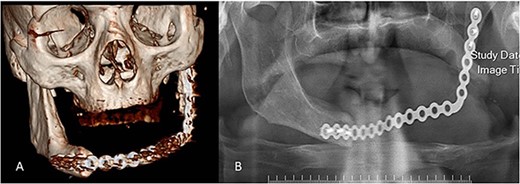
Postoperative radiographs. (A) 3D view of the reconstruction plate. (B) Panoramic view of the reconstruction plate after 24 months.
DISCUSSION
Oral pulse granuloma is a rare lesion of the oral cavity, which is characterized by the presence of giant cells and hyaline rings [2]. There are several reports of the presence of pulse granuloma in the lungs following the aspiration of certain materials, as well as in ulcerated or perforated areas of the gastrointestinal tract and rectum [6].
Histopathologically, it is recognized as irregular oval or spherical bodies surrounded by adjacent fibroblasts. In H&E staining, they are seen as homogenous eosinophilic material. Occasionally, they can be seen in the form of calcified round basophilic bodies within amorphous hyaline materials [3]. The exact etiology of oral pulse granuloma is debated, but in general, impaction of food residues through extraction sockets, deep periodontal pockets, untreated root canals and decayed teeth are considered possible etiological factors. The endogenous origin of this lesion is related to degenerative changes in blood vessel walls and collagen fibers [6].
Talacko believed that when vegetable seeds and food debris reach the body’s tissues, they are quickly digested and altered by host responses. The cellulosic part of the plant foods is indigestible and it became in the form of hyaline substances in the tissue. Finally, it produces chronic granulomatous reactions [7]. Harrison et al. proposed the vegetable nature theory for hyaline rings based on the ultrastructural investigation. They provide evidence that cellulose is the main component of hyaline rings; hence, the name oral vegetable granuloma was considered [8]. Oral pulse granuloma has been reported to be more common in the posterior mandible because the accumulation and retention of food often occur in this area [9].
In a study conducted by Chen et al., the hyaline bodies found in the connective tissue were examined and the authors explained the stages of hyaline ring formation. The first step is the pooling and coagulation of extravasated serum proteins in areas of previous trauma or chronic inflammation, the second step is the formation of a coagulum of proteins and ring arrangement around it and finally, the solidification of the hyaline rings thus causing entrapment [9]. According to previous studies (Table 1), the required histopathological criteria for diagnosing oral pulse granuloma include circular homogenous or fibrillar masses of eosinophilic hyaline rings, chronic inflammatory reaction and giant cells indicator of a foreign body [2].
| Author . | Number of cases . | Location . | Age (year) . | Gender (F/M) . | Duration (months) . | Symptoms . | Extraoral swelling . | Treatment . | Recurrence . |
|---|---|---|---|---|---|---|---|---|---|
| Harry H. Mincer (1979) | 4 | Mandible | 49–69 | M | N.M | Pain No symptoms | N.M | Surgical excision | N.M |
| M. D. McMillan (1981) | 3 | Mandible | 38/43/62 | F M | Discomfort Pus | No | Surgical excision | N.M | |
| Harrison JD (1986) | 10 | Mandible | 16–65 | M F | 2–10 | Pain N.M | N.M | Surgical excision | N.M |
| Brown et al. (1987) | 1 | Mandible | 65 | F | 18 | Tenderness | NO | Surgical excision | NO |
| Laisheng Chou (1990) | 1 | Mandible | 55 | M | 72 | Discomfort | Yes | excision | Yes |
| Gowda BK et al. (2011) | 1 | Mandible | N.M | F | N.M | Pain and swelling | No | excision | No |
| Author . | Number of cases . | Location . | Age (year) . | Gender (F/M) . | Duration (months) . | Symptoms . | Extraoral swelling . | Treatment . | Recurrence . |
|---|---|---|---|---|---|---|---|---|---|
| Harry H. Mincer (1979) | 4 | Mandible | 49–69 | M | N.M | Pain No symptoms | N.M | Surgical excision | N.M |
| M. D. McMillan (1981) | 3 | Mandible | 38/43/62 | F M | Discomfort Pus | No | Surgical excision | N.M | |
| Harrison JD (1986) | 10 | Mandible | 16–65 | M F | 2–10 | Pain N.M | N.M | Surgical excision | N.M |
| Brown et al. (1987) | 1 | Mandible | 65 | F | 18 | Tenderness | NO | Surgical excision | NO |
| Laisheng Chou (1990) | 1 | Mandible | 55 | M | 72 | Discomfort | Yes | excision | Yes |
| Gowda BK et al. (2011) | 1 | Mandible | N.M | F | N.M | Pain and swelling | No | excision | No |
| Author . | Number of cases . | Location . | Age (year) . | Gender (F/M) . | Duration (months) . | Symptoms . | Extraoral swelling . | Treatment . | Recurrence . |
|---|---|---|---|---|---|---|---|---|---|
| Harry H. Mincer (1979) | 4 | Mandible | 49–69 | M | N.M | Pain No symptoms | N.M | Surgical excision | N.M |
| M. D. McMillan (1981) | 3 | Mandible | 38/43/62 | F M | Discomfort Pus | No | Surgical excision | N.M | |
| Harrison JD (1986) | 10 | Mandible | 16–65 | M F | 2–10 | Pain N.M | N.M | Surgical excision | N.M |
| Brown et al. (1987) | 1 | Mandible | 65 | F | 18 | Tenderness | NO | Surgical excision | NO |
| Laisheng Chou (1990) | 1 | Mandible | 55 | M | 72 | Discomfort | Yes | excision | Yes |
| Gowda BK et al. (2011) | 1 | Mandible | N.M | F | N.M | Pain and swelling | No | excision | No |
| Author . | Number of cases . | Location . | Age (year) . | Gender (F/M) . | Duration (months) . | Symptoms . | Extraoral swelling . | Treatment . | Recurrence . |
|---|---|---|---|---|---|---|---|---|---|
| Harry H. Mincer (1979) | 4 | Mandible | 49–69 | M | N.M | Pain No symptoms | N.M | Surgical excision | N.M |
| M. D. McMillan (1981) | 3 | Mandible | 38/43/62 | F M | Discomfort Pus | No | Surgical excision | N.M | |
| Harrison JD (1986) | 10 | Mandible | 16–65 | M F | 2–10 | Pain N.M | N.M | Surgical excision | N.M |
| Brown et al. (1987) | 1 | Mandible | 65 | F | 18 | Tenderness | NO | Surgical excision | NO |
| Laisheng Chou (1990) | 1 | Mandible | 55 | M | 72 | Discomfort | Yes | excision | Yes |
| Gowda BK et al. (2011) | 1 | Mandible | N.M | F | N.M | Pain and swelling | No | excision | No |
In an attempt to explain the endogenous origin of oral pulse granuloma, it was hypothesized that collagen fibers are degenerated by giant cells and inflammatory cells originate from hyaline rings, and finally, macrophages and giant cells secrete collagen fibers against the secretion of specific enzymes. There are changes in collagen structure and hyaline rings’ appearance [8].
Talacko et al. [7] conducted a retrospective study and found evidence of pulse granuloma incidence in relation to periapical lesions and odontogenic cysts, which were missed initially at the time of diagnosis. In a similar retrospective study on inflammatory odontogenic cysts conducted by Henriques et al. [10], only 3.3% (22 of 661 cases) of inflammatory cysts were associated with oral pulse granuloma. This explains why OPG is a diagnosis that is rarely clinically suspected by clinicians.
In the case we presented, these histopathological criteria were present and eventually led to the diagnosis of oral pulse granuloma. Final treatment includes complete excision of the lesion and then a follow-up of the patient and monitoring for recurrence.
In conclusion, oral pulse granuloma is a rare lesion of unknown etiology. Diagnosis of this lesion is possible only by microscopic examination and has no pathognomonic clinical or radiographic appearance. Further studies on the nature of this lesion and the process of its formation are recommended.
ACKNOWLEDGEMENTS
The authors would like to thank the patient for giving consent for the publication of the case.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted without any commercial or financial relationships construed as a potential conflict of interest.
FUNDING
The study was not funded.
ETHICAL APPROVAL
No ethical approval is required.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal’s patient consent policy.
GUARANTOR
Dr Kimia H. Motlagh, postgraduate student, Department of Oral Medicine, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.



