-
PDF
- Split View
-
Views
-
Cite
Cite
Anand Marya, Jitendra Sharan, Prasad Mandava, El-Hassanein Hussein El-hassanein, Complications associated with the surgical removal of non-syndromic supernumerary premolar tooth buds in the mandible, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad304, https://doi.org/10.1093/jscr/rjad304
Close - Share Icon Share
Abstract
Hyperdontia involving the premolar teeth can be single or multiple or even related to a syndrome. These are frequently encountered in permanent dentition, but their occurrence has ranged between 0.09 and 0.64% in the general population. These are commonly found between the permanent canines and first premolars but rarely between the first and second premolars. These are usually eumorphic and can be easily identified as they follow the conventional tooth morphology. These are usually asymptomatic and not easily palpable unless they are very close to eruption. A lingual approach is preferred during their removal over the buccal method as it poses less risk of root trauma. In this case, bilateral accessory premolar tooth buds were present between the first and second premolars. Since the patient was undergoing orthodontic treatment, she was advised to remove these accessory teeth. For their removal, a Neumann flap with a buccal approach was used, which led to fracturing the root apex of the mandibular right second premolar root. On follow-up over the next 1 year, no other complications or secondary tooth germs were observed, and following a period of bone formation, the bone in the affected area formed normally again.
INTRODUCTION
The prevalence of non-syndromic supernumerary premolars in the general population is 0.09–0.64%, making it rare [1, 2]. Mandibular premolars are commonly recognized as the supernumerary teeth most challenging to extract due to the high density of the lower jaw bone, proximity to the mental nerve on the buccal side and lack of direct visualization from the lingual aspect [3].
CASE REPORT
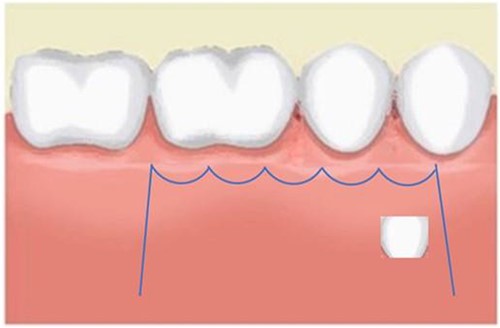
A 21-year-old patient with a non-contributory history reported to the clinic with a complaint of spacing in the anterior teeth. On radiographic examination, eumorphic supernumerary premolar crowns were found located between the roots of the mandibular first and second premolars (Fig. 1). The patient was completely asymptomatic and had no knowledge regarding the presence of these accessory teeth.

Image depicting the supernumerary premolar buds located between the first and second mandibular premolars.
A Neumann full-thickness buccal flap was utilized to remove these during the course of orthodontic treatment. The shortcoming of the buccal surgical removal approach is that although it is better for visualization, it poses a high risk of trauma to the adjacent teeth or nerves [4, 5]. As the premolar was being removed on the right side, there was a fracture of the root apex (Fig. 2). On the left side, the premolar bud could be removed without any trauma to the adjacent tooth roots. After months of follow-up, there was normal bone formation, and no other symptoms were identified (Fig. 3).

Follow-up panoramic 1 week after removal of the supernumerary premolars.

Follow-up panoramic image 1-year after removal of the supernumerary premolars.
DISCUSSION
In this case, the bilaterally present supernumerary premolars presented as an obstruction to tooth movement; therefore, it was essential to have them removed. Surgical removal of these impacted teeth may involve the risk of damage to adjacent roots/ structures, and the patient must be made aware of these risks before a decision is made to remove these supernumerary premolars surgically.
In this context, a buccal approach using a Neumann full-thickness flap was preferred (Fig. 4). When a buccal approach is planned, then the location of the mental nerve must be identified to avoid any post-operative sensory problems. The most challenging part is to exercise extreme caution during Ostectomy to avoid damage to the adjacent tooth roots.
CONCLUSION
The non-syndromic presence of para-premolars is rare, and while radiographic diagnosis is essential to identify the position, the surgical approach to remove these premolars must be precise. In some instances, the premolars may be left in place, but in this case, since the patient was receiving fixed orthodontic treatment and involved tooth movement in that region, it was decided to remove the accessory premolar tooth buds surgically. This case is a good example of both the success and the problems with surgically removing the additional premolars using the Neumann flap approach.
ACKNOWLEDGMENTS
The authors would like to thank the patient for giving their consent.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY STATEMENT
Any data related to the study can be provided on reasonable request from the corresponding author.
AUTHORS' CONTRIBUTIONS
AM: patient treatment AM: diagnosis and treatment planning AM: manuscript preparation, AM, PM, EHEH and JS: review and editing.
PATIENT CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal’s patient consent policy.



