-
PDF
- Split View
-
Views
-
Cite
Cite
Hiroshi Shiratori, Takanobu Onoda, Naoki Takabayashi, Chika Harada, Sae Imada, Yusuke Kita, Shinsuke Kazama, Yukio Ishihara, Ryo Kobayashi, Takeyuki Hiramatsu, Laparoscopic repair for internal hernia associated with colostomy: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad290, https://doi.org/10.1093/jscr/rjad290
Close - Share Icon Share
Abstract
A 63-year-old woman was admitted with abdominal pain two months after laparoscopic abdominoperineal resection for rectal cancer. Computed tomography revealed dilated small intestine had passed through a defect between the lifted sigmoid colon and abdominal wall. She was diagnosed with small bowel obstruction without strangulation due to internal hernia and managed nonoperatively based on her wish. Recurrence of intestinal obstruction occurred for which curative surgery was performed laparoscopically. The herniated intestine was restored to the normal position, and the hernia orifice was closed using barbed suture, on laparoscopic management. Internal hernia is a rare complication after colostomy that requires surgical management. Although laparoscopic approach on re-operation is difficult, laparoscopic surgery may be suitable for patients with IHAC in terms of required less use of adhesiolysis.
INTRODUCTION
Internal hernia is a rare complication after gastrointestinal surgery. However, it may cause life-threatening conditions such as bowel strangulation or perforation. The incidence of symptomatic internal hernia after laparoscopic colorectal surgery was reported to be 0.38–0.65% [1, 2]. The major cause of internal hernia after colorectal surgery is mesenteric defect [1]. When patients develop internal hernia, emergency surgery, including a closure of mesenteric gap, is required. Some studies demonstrated better outcomes using the laparoscopic approach compared to the open approach; however, the rate of conversion to open surgery is high [3, 4].
Abdominoperineal resection (APR) is performed for patients with rectal malignancies. A sigmoid colostomy on APR procedure is commonly passed through an intraperitoneal route. The lifted colostomy creates a new intraperitoneal space in the lateral side, which potentially causes an internal hernia. To date, there have been few reports describing internal hernia associated with colostomy (IHAC) in the lateral side of colostomy [5–7].
We herein describe a patient that developed IHAC after laparoscopic APR, who was successfully repaired laparoscopically.
CASE REPORT
A 63-year-old woman underwent laparoscopic APR for low rectal cancer in our institution. Sigmoid colostomy was created through an intraperitoneal route. The patient’s postoperative course was uneventful.
Two months after the surgery, the patent was admitted with moderate tenderness around the umbilicus during a course of adjuvant chemotherapy. Computed tomography revealed dilated small intestine in the lateral space of the lifted sigmoid colostomy with a caliber change adjacent to the left side of the lifted colostomy (Fig. 1). Neither closed loop nor reduced enhancement on the intestine was found. Small bowel obstruction resulting from adhesion or internal hernia associated with the lifted colostomy was suspected. Because her abdominal tenderness disappeared immediately after admission, the patient was managed nonoperatively and quickly recovered. One month later, recurrence of small bowel obstruction occurred, which quickly improved in a similar manner to the last hospitalization. Curative surgery was recommended but not scheduled based on the patient’s wish. However, recurrence of the intestinal obstruction was occurred repeatedly. Finally, curative surgery for repeated small bowel obstruction was scheduled seventeen months after the first occurrence. Laparoscopic surgery was performed using three ports, which were placed on the epigastric, right-upper and right-lower quadrant areas (Fig. 2a). Laparoscopy revealed that the small intestine had passed through a defect between the lifted sigmoid colon and abdominal wall in a cranial-to-caudal direction (Fig. 2b). There were no findings of dilatation and adhesion in the herniated intestine, which was easily restored to the normal position. The hernia orifice between the lifted sigmoid colon and lateral wall was closed by running suture to prevent recurrent herniation (Fig. 2c and d). To prevent loosening of the suture line, barbed suture was used for closing the enlarged hernia orifice. The patient’s postoperative course was uncomplicated, and she was discharged on the fifth day after the second surgery.
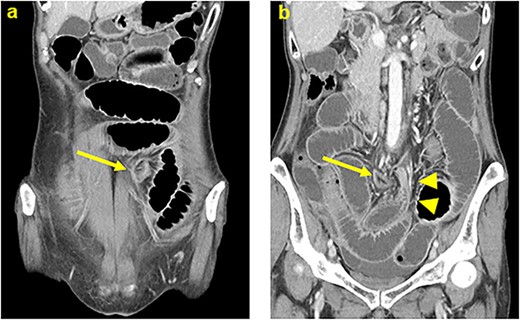
Computed tomography showed that dilated small intestine were positioned in the lateral space of the lifted sigmoid colostomy. (a) A caliber change of dilated intestine was found adjacent to the left side of the lifted colostomy (b). Arrows: the lifted sigmoid colostomy; arrowheads: a caliber change of the dilated intestine.
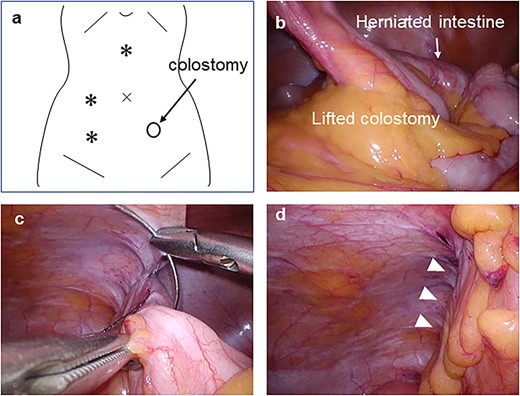
Laparoscopic surgery was performed using three ports (a). Small intestine had passed through a defect between the lifted sigmoid colon and abdominal wall in a cranial-to-caudal direction (b). The hernia orifice between the lifted sigmoid colon and lateral wall was closed using barbed suture (c and d). *: port placement; arrowheads; suture line of hernia orifice closure.
DISCUSSION
Major complications after colostomy include stoma stenosis, leakage, prolapse, parastomal hernia, retraction and intestinal obstruction, which occur in 21–70% of patients [8]. The major cause of intestinal obstruction is intraperitoneal adhesion, and a minor cause is internal hernia to the mesenteric gap. IHAC is a rare complication after colostomy [5–7].
The laparoscopic approach was reported to be a risk factor for post-operative internal hernia on gastrointestinal surgery, which was associated with less adhesion [9, 10]. In previous reports of IHAC, similar to the present case, most cases were managed laparoscopically on primary surgery of rectal cancer. Thus, patients after laparoscopic APR may be more likely to develop IHAC compared with open APR.
In patients with adhesive small bowel obstruction, several studies demonstrated the improved postoperative outcome of laparoscopic adhesiolysis compared to the open technique in terms of length of hospital stay and morbidity [3, 11]. According to these reports, patient selection was the key factor for success of laparoscopic approach. Especially in patients with severe and complex adhesions, the conversion rate was high. In addition, a high complication rate was found in the converted group [4]. Considering less adhesion in patients with IHAC, a herniated intestine could be easily restored to its normal position on laparoscopic surgery for IHAC, as with the present case. Reported methods of hernia closure are handsaw closure, omental patch and stoma revision via extraperitoneal route [5–7]. Handsaw hernia closure, which is a running suture between the peritoneum of the abdominal wall and lifted colostomy, is the simplest. Laparoscopic handsaw closure using a normal suture may be difficult because the elevated abdominal wall on laparoscopy can cause suture loosening. Using a barbed suture could have resolved the difficulty in the present case. Barbed sutures, which are used worldwide on laparoscopic surgery, are monofilament sutures with barbs that allow them to self-anchor. The design of the suture maintains tissue approximation without the need for surgical knots and constant tension on the suture line. On laparoscopic gastrointestinal anastomosis, using barbed sutures contributed to shorter operative time [12]. For IHAC repair, barbed sutures are effective in terms of not loosening the running suture.
The incidence of IHAC remains unclear. In a past study of mesenteric internal hernia, Daster et al. reported the incidence of asymptomatic internal hernia was 27% after laparoscopic colorectal surgery, suggesting a routine closure of mesenteric gap at the time of primary surgery [13]. This suggests that asymptomatic IHAC after laparoscopic APR may not be rare. Nationwide studies for clearing the incidence of IHAC are needed.
In conclusion, laparoscopic surgery for IHAC may be acceptable in terms of required less use of adhesiolysis. Using barbed sutures may reduce the difficulty of hernia closure.
CONFLICT OF INTEREST STATEMENT
We declare that there is no conflict of interests.
FUNDING
We declare that no funding was received in support of this work.
DATA AVAILABILITY
Data sharing is not applicable to this article as no new data were created or analyzed in this study.



