-
PDF
- Split View
-
Views
-
Cite
Cite
Andreea Sandica, Djawid Baraksei, Sabeth Hüsken, Richard Viebahn, Iurii Snopok, Pneumoperitoneum: always a surgical case?, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad250, https://doi.org/10.1093/jscr/rjad250
Close - Share Icon Share
Abstract
Spontaneous idiopathic pneumoperitoneum (SIP) is a rare condition in the surgical practice. We introduce a case of an alcoholic male who presented with nausea, vomiting and diarrhea without clinical signs of peritonitis. A computed tomography of the abdomen showed free air distributed mainly along the ascending colon. We performed an emergency laparoscopy, which revealed no signs of perforation or bowl ischemia but showed air bubbles in the mesentery along the ascending colon. Subsequent endoscopy revealed unclassified inflammatory bowel disease manifesting in the rectum, erythematous mucosa and epithelialized erosions of the stomach. The patient discharged himself on Day 8 after the surgery. The causes of SIP are unknown, but some authors assume microperforation. SIP can be a challenge for the choice of therapy. Laparoscopy may be particularly beneficial in patients with generalized peritonitis, while patients with moderate symptoms may benefit from conservative treatment.
INTRODUCTION
Spontaneous idiopathic pneumoperitoneum (SIP) is a rare condition, which does not always have to be a surgical case in the absence of clear symptoms and peritonitis. As it is a diagnosis by exclusion, many patients undergo unnecessary procedures that imply the risk of injuring hollow viscus without bringing real benefit to the patients. Here we present the case of a patient who was diagnosed with idiopathic pneumoperitoneum at our hospital, aiming to raise awareness of this condition and improve the management of similar findings.
CASE REPORT
A 55-year-old male was hospitalized by the Department of Gastroenterology with nausea and vomiting over the past 2 weeks. He also mentioned diarrhea starting 2 days before admission. Further medical history revealed alcoholism. On clinical examination, he showed moderate abdominal distention and normal bowel sounds. There was no sign of peritonitis. His body temperature was within normal range. Laboratory findings showed elevated levels of transaminases, alkaline phosphatase and bilirubin. White cell counts and C-reactive protein were within normal range. A computed tomography (CT) scan of the abdomen showed free air distributed along the ascending colon and above the liver with punctum maximum in the right upper quadrant (Fig. 1). The patient underwent an emergency laparoscopy, which revealed no sign of perforation or bowl ischemia but showed air embedment in the mesenterium along the ascending colon (Fig. 2). Subsequent coloscopy revealed an unclassified inflammatory bowel disease manifesting in the rectum. Gastroscopy showed erythematous mucosa and epithelialized erosions. Endosonography showed mild chronic pancreatitis without duct obstructions or pseudocysts. Sonography and endosonography of the liver and bile ducts showed signs of alcoholic steatohepatitis, confirmed by liver biopsy. The patient discharged himself on Day 8 after the surgery.
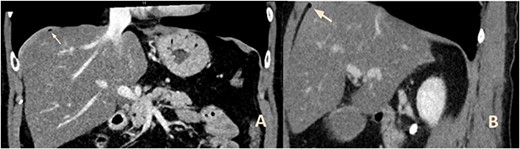
CT of the upper abdomen with frontal (a) and sagittal (b) reconstructions showing the air bubbles above the liver (arrows).
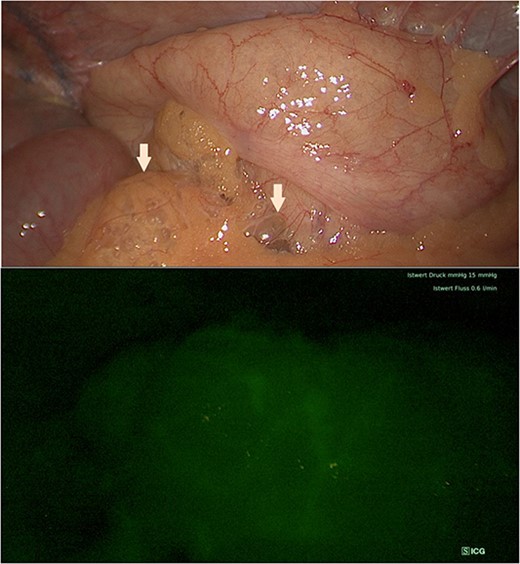
Intraoperative view showing air bubbles embedment in the mesenterium along the ascending colon (arrows) and indocyanine green fluorescence imaging of the bowel perfusion.
DISCUSSION
Nonsurgical pneumoperitoneum makes about 10% of the cases identified on CT- or X-ray scans. Publications as by Mularski et al. [1] classified possible causes of this condition using five categories: postoperatively retained air, thoracic, abdominal, gynecologic and idiopathic. Most cases presented until now in the English literature with SIP had preexistent conditions like chronic obstructive pulmonary disease, peptic ulcera, suffered from sepsis, had been medicated with steroids or had undergone chemotherapy. Our patient had a history of alcoholism and freshly epithelialized erosions found on gastroscopy, as well as a chronic pancreatitis and steatohepatitis. However, the cause of the diagnosed pneumoperitoneum could not be identified with certainty in neither of these patients. In this context, Mularski et al. [1] suggested that a subclinical microperforated hollow viscus may have been present prior to negative laparotomy or laparoscopy in SIP. Such a leak must be small enough to permit the escape of gas without the evolution of bowel contents, and it must occur in a patient whose resistance to infection is intact. In the case of our patient, this might have been caused by an inflammatory bowel disease as found on coloscopy or peptic erosions as found on gastroscopy. Upon admission there were no clinical signs pointing towards perforated viscus to correspond with the radiological results. The performed laparoscopy also remained negative for perforated viscus.
Most of the patients with SIP experienced either mild symptoms upon admission like our patient or were incidentally diagnosed with this condition and treated with antibiotics and fluids [1–5]. In the publication of Valez, the patient presented with emesis and abdominal pain showing moderate abdominal distension and leukocytosis upon work-up. He underwent diagnostical laparoscopy, which was converted to laparotomy with resection of a pneumatosis-like changed bowel. Postoperatively, he developed symptoms of an ileus, which resolved conservatively. Two years later, he returned to the hospital with recurrent SIP and was again taken for a diagnostic laparoscopy with no result [2]. McLaren published another case presenting with moderate distension of the abdomen and normal bowel movements who was taken for a laparoscopy after pneumoperitoneum showed on X-ray scans without sign of perforation. After surgery, the patient went into ileus with rising infection parameters needing a nasogastric tube [3]. Both experiences come to show that a radical approach can worsen the patients’ condition when there is no sign of peritonitis or infection to correlate with the pneumoperitoneum diagnosed radiologically. Grewal et al. [4] presented another case of a patient with SIP who was admitted with relevant abdominal tenderness and underwent diagnostic laparoscopy. The symptoms resolved after surgery and were not recurrent on follow-up.
Further cases published by Woelfel et al. [6] as well as Jones et al. [7] identified a developing spontaneous bacterial peritonitis as the cause of spontaneous pneumoperitoneum. Both patients had a history of alcoholism, cirrhosis and underwent laparoscopy without sign of perforated hollow viscus like in the patient we have treated. Microbiology revealed gram-negative bacteria and Clostridium perfingens, respectively. We could not isolate pathogen bacteria or identify the cause of the infection in our case but found signs of colitis upon endoscopy as described above.
SIP is a rare disease that has only been addressed a few times in the English literature up to this point. Being a rare condition, it represents a challenge to surgeons regarding the choice of therapy. Experience shows that diagnostic laparoscopy can be beneficial to such patients especially facing generalized peritonitis. It has been shown that patients admitted with moderate symptoms and no signs of infection can be primarily observed and have a better course if a conservative line of treatment is followed [8, 9]. In patients with risk factors for perforation of hollow organs, it is important to exclude such a complication, which can also be done by endoscopy if the patient’s condition permits [5, 8, 9].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.



