-
PDF
- Split View
-
Views
-
Cite
Cite
Halit Maloku, A rare case report: low grade appendiceal mucinous neoplasm (LAMN) located under the left costal margin, the gastric level and the transverse colon, Journal of Surgical Case Reports, Volume 2023, Issue 5, May 2023, rjad234, https://doi.org/10.1093/jscr/rjad234
Close - Share Icon Share
Abstract
We report a case with a low-grade appendiceal mucinous neoplasm, located under the left costal margin, the gastric level and the transverse colon. The mucinous appendiceal neoplasm has caused intussusception of the appendix in the cecum, completely dislocating the cecum on the left side of the upper abdomen. In such cases, it is important to diagnose prior to surgical treatment to avoid mucocele perforation and intraoperative dissemination. The patient underwent a right hemicolectomy procedure, completely removing the mass according to oncological principles. The atypical localization of the cecum leads to difficulty in diagnosing the mucinous neoplasm of the appendix. It is important to know the diagnosis before the operation to plan the right course of treatment.
INTRODUCTION
We report a case with low-grade appendiceal mucinous neoplasm (LAMN), located under the left costal margin, the gastric level and the transverse colon.
LAMN are rare neoplasms that arise from the appendix, with an incidence of ~0.2–0.6 cases per 100 000 individuals per year. They can cause symptoms like stomach pain, bloating and changes in bowel movements by causing a buildup of mucus in the appendix. Usually, doctors find LAMNs during appendectomy.
The clinical presentation of mucinous neoplasms is atypical. Diagnosing with CT or MRI is recommended for adequate treatment and avoidance of intraoperative dissemination such as pseudomyxoma peritonei, which has a high mortality rate.
In the CT, the lesion is described by the radiologist as a suspicion for mesenteric formation on the upper left side of the abdomen, whereas in MRI, it is described as the intussusception of the transverse colon. During the surgery, an appendiceal mucinous neoplasm is seen, with cecum ectopy under the left costal margin, the gastric level and the transverse colon. The cecum ectopy may be the cause of inaccurate diagnostics by the radiologist.
CASE PRESENTATION
A 42-year-old female patient is admitted in the emergency department because of severe abdominal pain located under the left costal margin, nausea and general fatigue. These complaints are more intense the last 3 days. In the last 6 months, she has experienced pronounced intestinal peristalsis localized in the upper left abdomen.
On the physical examination, a mass is palpated under the left costal margin, with a diameter of 6 cm. Routine laboratory tests result in mild leukocytosis of 10.2 and a slightly increased C-reactive protein of 15. The patient denies having any accompanying diseases. An abdominal CT and MRI with contrast are performed.
After reviewing the abdominal CT with contrast, the radiologist has reached the conclusion that there is a suspicion of a ‘mesenteric formation’ (Fig. 1).
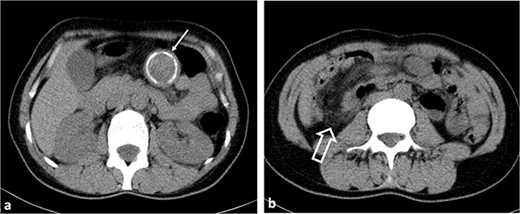
Axial non-contrast CT images. (a) A hypodense lesion (thin arrow) with peripheral calcification is observed in the left upper quadrant of the abdomen. (b) Ileocolic intussusception is observed in the right lower quadrant of the abdomen (thick arrow).
The radiologist’s description of the abdominal MRI with contrast has led to a suspicion of ‘intussusception’ in the transverse colon (Figs 2 and 3).
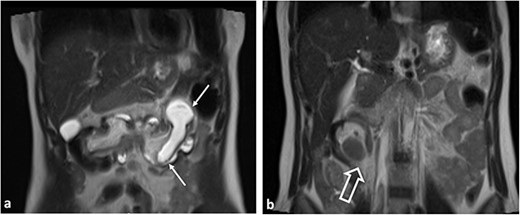
Coronal T2WI MR images. (a) Tubular lesion (thin arrow) consistent with hyperintense appendiceal mucocele is observed in the left upper quadrant of the abdomen. (b) Ileocolic intussusception is observed in the right lower quadrant of the abdomen (thick arrow).
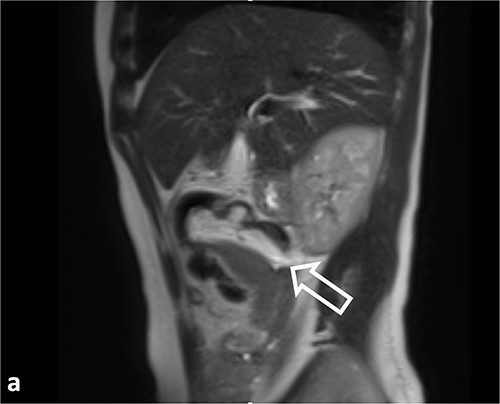
Sagittal T2WI MR images. Ileocolic intussusception (thick arrow).
Because of the presence of a sizable mass under the left costal margin and concern for malignancy, the patient underwent urgent surgery via a supraumbilical median laparotomy.
While performing the surgery, the surgical team observed a neoplastic mass at the base of the appendix, measuring 6 cm in diameter. The mass was causing an obstruction of the appendix, which had expanded to dimensions of 8 × 2.5 cm and extended intraluminally up to the ileocecal valve. Right hemicolectomy and ileo-colon transverse T–T anastomosis are performed (Fig. 4).
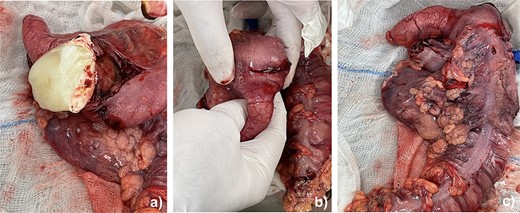
The neoplasm mass along with right colon, ileum and the appendix. (a) Mucinous neoplasm of the appendix. (b) Intussusception of the base of the appendix in the cecum. (c) Right hemicolectomy.
The surgery was successful, and the patient’s postoperative condition was favorable. They were discharged in good health and returned home on the 70th day after the procedure.
The histopathological examination showed that the patient had a LAMN. Additionally, reactive lymph nodes were found in the pericolic and mesenteric adipose tissue, with the largest measuring 10 mm in diameter.
Following the diagnosis, the patient consulted with an oncologist and underwent the necessary laboratory and imaging examinations as per protocol. As of today, the patient is in good health.
DISCUSSION
Diagnosis is often incidental or intraoperative finding at resection for suspicion of appendicitis. Appendiceal mucinous neoplasm is commonly misdiagnosed as acute appendicitis, adnexal mass or retroperitoneal neoplasms [1]. While CT imaging suggested it was a mesenteric neoplasm, and MRI imaging indicated intussusception of the transverse colon, intraoperative examination revealed a neoplasm of the appendix with histopathology confirming LAMN. Timely identification and treatment of LAMN is crucial for reducing PMP risk and improving prognosis and outcome [2]. In our case, the intervention was performed at the right time, without the presence of malignant cells in the abdominal fluid and mesenteric lymphatic vessels. Traditionally, they are diagnosed by radiologic imaging or identified intraoperatively; however, rarely, they may be diagnosed during an endoscopic procedure [3]. Their diagnosis may pose challenges in clinical, radiological, and pathological identification, particularly as they may be mistaken for gynecological pathologies in females [4]. In our case, the localization was atypical, in the upper left epigastrium. A rare case with intussusception is described, that is caused by either intestinal hemangiomas or appendiceal mucinous neoplasms [5]. In our case, the intussusception was caused by the appendiceal mucinous neoplasm. It should be noted that PMP can occasionally be accompanied by rectal cancer [6]. In some instances, neoplasm of the appendix may be accompanied by other malignant diseases, such as rectal cancer, but in our patient, only LAMN was present.
CONCLUSION
Prompt diagnosis and timely treatment of mucinous neoplasms of the appendix are critical to prevent rupture and the subsequent development of high mortality pseudomyxoma peritonei. It is important to note that atypical localization of the appendix, such as in the upper abdomen under the left costal margin, should be considered, even though such cases are very rare.
The challenging nature of diagnosing mucinous neoplasms before surgical intervention, as in our case (where CT indicated a mesenterial formation and MRI indicated intussusception of the transverse colon), highlights the importance of preoperative diagnosis in establishing appropriate treatment during surgery. Mucinous neoplasms because of the deposition of calcium salts in the mucin give the appearance of calcified ring, which has not been described previously in literature.
When mucinous neoplasms of the appendix are suspected, a hemicolectomy is preferred, as was done in our case, to avoid the possibility of intraperitoneal iatrogenic dissemination.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
The data is included in the manuscript itself.



