-
PDF
- Split View
-
Views
-
Cite
Cite
So Kasuga, Shinya Abe, Hiroaki Nozawa, Kazuhito Sasaki, Koji Murono, Shigenobu Emoto, Hiroyuki Matsuzaki, Yuichiro Yokoyama, Yuzo Nagai, Yuichiro Yoshioka, Takahide Shinagawa, Hirofumi Sonoda, Tetsuo Ushiku, Soichiro Ishihara, Diverticular perforation of terminal ileum associated with chemotherapy for non-small cell lung carcinoma: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad179, https://doi.org/10.1093/jscr/rjad179
Close - Share Icon Share
Abstract
A 71-year-old man was diagnosed with advanced non-small cell lung carcinoma and treated with chemotherapy developed ileocecal diverticulitis three times over the last 2 months of receiving second-line treatment. During the fourth diverticulitis event, the patient presented with fever and abdominal pain, worsening after 5 days. Abdominal computed tomography showed ascites and intra-abdominal free air, suggesting bowel perforation with acute diffuse peritonitis. We performed emergency surgery; the surgical findings showed diverticulosis with perforated diverticula in the ileocecal region. We performed ileocecal resection, an ileostomy and a mucous fistula of the ascending colon. Histopathological examinations revealed pseudodiverticula at the perforation, where the mucosa was depressed through the muscularis propria. Hence, we diagnosed perforated ileal diverticulitis. Repeated diverticulitis triggered by chemotherapy might have resulted in perforation. Small bowel diverticula are rare, but diverticulitis can occur in patients receiving chemotherapy and with cases of unexplained fever and abdominal pain.
INTRODUCTION
Colon diverticulosis is common, with a prevalence of ~42–60% [1–3], whereas small intestine diverticulosis, excluding Meckel’s diverticula, is rare, affecting 0.02–7%. Ileal diverticulosis is less common than jejunum diverticulosis. Small intestine diverticulosis is often asymptomatic and detected only during imaging or autopsy [1, 4].
This case reports a small intestinal diverticular perforation in a patient receiving chemotherapy for non-small cell lung cancer. Immunocompromised patients taking methotrexate or steroids or receiving chemotherapy are at a higher risk of developing severe diverticulitis that may not respond to conservative treatment [6–8]. Chemotherapy patients also face significantly higher perforation risk [8]. This is reportedly the first case of ileal diverticulitis perforation in a chemotherapy patient.
CASE REPORT
A 71-year-old man was diagnosed with advanced non-small cell lung carcinoma and pleura and lymph node metastasis. He received carboplatin, paclitaxel, bevacizumab and atezolizumab every 3 weeks as first-line chemotherapy for 4 months. As the pleural dissemination worsened, docetaxel and ramucirumab were administered as second-line treatment. The patient had three episodes of ileocecal diverticulitis following chemotherapy, all of which were treated conservatively with antimicrobials and fasting therapy. The diverticulitis episodes and computed tomography (CT) images are shown in Figs 1 and 2a–c. During the fourth diverticulitis episode, the patient presented with fever and abdominal pain, worsening after 5 days. Physical examination revealed tenderness and rigidity throughout the abdomen. Vital signs were stable, but body temperature was 37.7°C. Laboratory data showed inflammation with a white blood cell (WBC) count of 21 400/μL and a C-reactive protein (CRP) level of 23.8 mg/dL. Abdominal CT imaging showed ascites and intra-abdominal free air around the right-side colon (Fig. 3). Hence, we suspected a right-side colon perforation with acute diffuse peritonitis and performed an emergency laparotomy with a midline incision. Surveying the small bowel revealed that ileal perforation occurred only a few centimeters proximal to the ileocolic valve (Fig. 4). The patient underwent ileocecal resection, ileostomy and a colonic mucous fistula.

Flowchart showing the trend of WBC count and CRP level from second-line chemotherapy to surgery. CTRX, ceftriaxone; PIPC/TAZ, piperacillin/tazobactam; MEPM, meropenem.
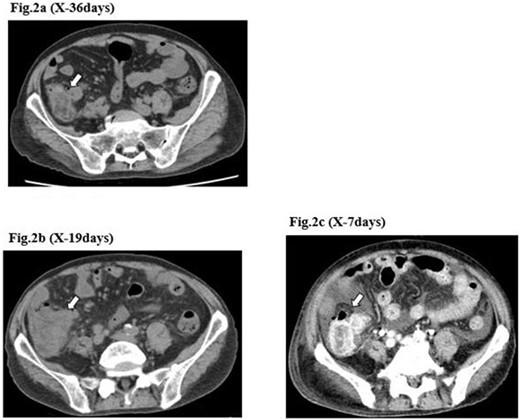
CT image of the ileocecal diverticulitis. The image shows that ileocecal diverticulitis (arrows) has occurred three times (a–c) until the diverticular perforation.

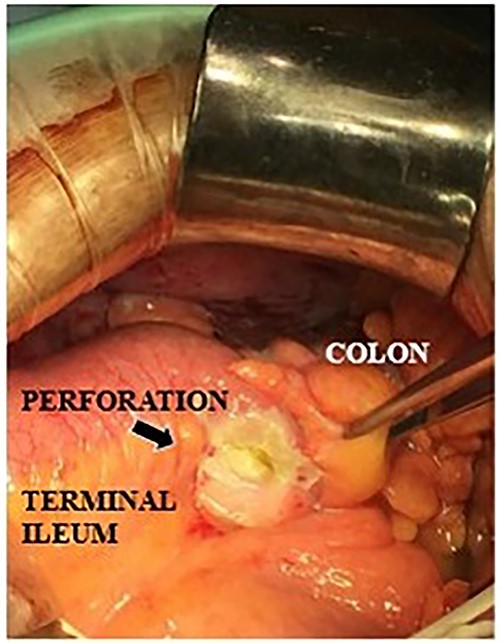
Intraoperative findings of a terminal ileal perforation on the mesenteric side (arrow).
The surgically resected specimen is shown in Fig. 5. Macroscopic findings indicated multiple ileal diverticula, with one perforated on the mesenteric border. Histopathological examinations revealed a pseudodiverticulum at the perforation where the mucosa was depressed through the muscularis propria. Additionally, inflammatory cell infiltration with abscess formation penetrating the serous surface was observed (Fig. 6).
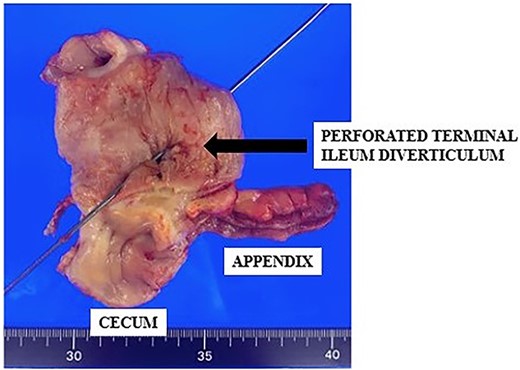
Resected specimen of ileocecum with the perforation of the terminal ileum (arrow).

Specimen cross-section and microscopic examination (hematoxylin and eosin staining) of the terminal ileal diverticula (arrow) and perforation site (arrowheads).
The postoperative course was uneventful, and the patient was discharged 24 days after surgery. The patient did opt for chemotherapy again and died about 6 months after the surgery.
DISCUSSION
Small bowel diverticulosis is rare, accounting for 0.02–7.1% of small bowel diverticulosis cases on imaging studies [4, 5] and 0.6–4.6% of autopsy cases [9, 10]. Reportedly, 80% of small intestinal diverticula are located in the jejunum, 15% in the ileum and 5% in both [10]. They are usually asymptomatic, but 30% are accompanied by chronic symptoms such as indigestion or irritable bowel syndrome-like symptoms, and only 10% are accompanied by inflammation, perforation, bleeding or obstruction [9, 10]. The small intestinal diverticulitis mortality rate is 21–45% because of low diagnostic rates and delayed treatment [10–12]. Diagnosing small intestinal diverticulitis may be difficult because of its rare occurrence. The small intestine’s location and free air may depend on body position and intestinal peristalsis, making it challenging to identify the perforation site and complicating imaging diagnosis, especially with extensive gut inflammation. Small intestine diverticula mostly occur on the mesenteric side because of the straight artery flowing into the tract, making it susceptible to diverticula.
Diverticula are more common in the jejunum than the ileum because of the large straight artery in the proximal jejunum, which promotes diverticula formation [9]. The patient had 2 months of repeated diverticulitis before the diverticula perforated, indicating weakened tissue from inflammation in the same area of the right colon to the ileum. Perforation and abscess risk may increase with each recurrence of colonic diverticulitis, but this is not documented in small bowel diverticulitis [13, 14]. No abscess or perforation was found in this case, and the patient was able to receive conservative care while continuing lung cancer treatment.
We conducted a MEDLINE search using the keywords ‘ileal diverticula’ and ‘perforation’ to identify previously reported cases of ileal diverticula perforation. Eight reports of diverticular penetration/perforation occurred exclusively in the ileum (Table 1) [4, 15–21], including one patient immunosuppressed by steroids. There was no chemotherapy-related case like the present case. Only one patient had a correct preoperative diagnosis. Seven of the eight patients underwent intestinal anastomosis, and only one underwent ileostomy, as in this case. Our patient was immunocompromised because of anticancer drug administration. As the patient had repeated diverticulitis episodes, the intestinal tract condition was weakened because of high inflammation, requiring creating an ileostomy to avoid complications related to the anastomosis.
Literature review of ileal diverticular perforation (excluding Meckel’s diverticula and cases of penetration)
| No . | Reference . | Year . | Age/ sex . | Past medical history . | Medication . | Preoperative diagnosis . | Perforation site . | Management . | Cause of perforation . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Miller et al. [16] | 1970 | 49/M | NA | NA | Appendicitis | Mesenteric border | Ileocecal resection | NA |
| 2 | Ackerman [17] | 1974 | Appendectomy Inguinal hernia Heart failure | Various medication | Sigmoid diverticulitis | Mesenteric border | Right hemicolectomy | Diverticulitis | |
| 3 | Roses et al. [5] | 1976 | 30/M | NA | NA | NA | Mesenteric border | Segmental ileal resection | Diverticulitis |
| 4 | Grana et al. [18] | 2009 | 75/M | NA | NA | Penetration of terminal ileum | NA | Right hemicolectomy | Diverticulitis |
| 5 | Kothadia et al. [19] | 2015 | 65/M | Hypertension Angina | NA | Sigmoid diverticulitis | NA | Elective surgery (Surgical technique was not described) | Diverticulitis |
| 6 | Thilakawardana et al. [20] | 2017 | 29/M | Acute renal failure | Steroids | NA | Segmental ileal resection | Diverticulitis | |
| 7 | Ramzee et al. [21] | 2020 | 69/M | NA | NA | Ileal diverticulitis | Mesenteric border | Segmental ileal resection Double-barrel ileostomy | NA |
| 8 | Saijo et al. [22] | 2020 | 55/M | NA | NA | Penetration of terminal ileum | Mesenteric border | Ileocecal resection | Diverticulitis |
| No . | Reference . | Year . | Age/ sex . | Past medical history . | Medication . | Preoperative diagnosis . | Perforation site . | Management . | Cause of perforation . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Miller et al. [16] | 1970 | 49/M | NA | NA | Appendicitis | Mesenteric border | Ileocecal resection | NA |
| 2 | Ackerman [17] | 1974 | Appendectomy Inguinal hernia Heart failure | Various medication | Sigmoid diverticulitis | Mesenteric border | Right hemicolectomy | Diverticulitis | |
| 3 | Roses et al. [5] | 1976 | 30/M | NA | NA | NA | Mesenteric border | Segmental ileal resection | Diverticulitis |
| 4 | Grana et al. [18] | 2009 | 75/M | NA | NA | Penetration of terminal ileum | NA | Right hemicolectomy | Diverticulitis |
| 5 | Kothadia et al. [19] | 2015 | 65/M | Hypertension Angina | NA | Sigmoid diverticulitis | NA | Elective surgery (Surgical technique was not described) | Diverticulitis |
| 6 | Thilakawardana et al. [20] | 2017 | 29/M | Acute renal failure | Steroids | NA | Segmental ileal resection | Diverticulitis | |
| 7 | Ramzee et al. [21] | 2020 | 69/M | NA | NA | Ileal diverticulitis | Mesenteric border | Segmental ileal resection Double-barrel ileostomy | NA |
| 8 | Saijo et al. [22] | 2020 | 55/M | NA | NA | Penetration of terminal ileum | Mesenteric border | Ileocecal resection | Diverticulitis |
M, male; F, female; NA, not available.
Literature review of ileal diverticular perforation (excluding Meckel’s diverticula and cases of penetration)
| No . | Reference . | Year . | Age/ sex . | Past medical history . | Medication . | Preoperative diagnosis . | Perforation site . | Management . | Cause of perforation . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Miller et al. [16] | 1970 | 49/M | NA | NA | Appendicitis | Mesenteric border | Ileocecal resection | NA |
| 2 | Ackerman [17] | 1974 | Appendectomy Inguinal hernia Heart failure | Various medication | Sigmoid diverticulitis | Mesenteric border | Right hemicolectomy | Diverticulitis | |
| 3 | Roses et al. [5] | 1976 | 30/M | NA | NA | NA | Mesenteric border | Segmental ileal resection | Diverticulitis |
| 4 | Grana et al. [18] | 2009 | 75/M | NA | NA | Penetration of terminal ileum | NA | Right hemicolectomy | Diverticulitis |
| 5 | Kothadia et al. [19] | 2015 | 65/M | Hypertension Angina | NA | Sigmoid diverticulitis | NA | Elective surgery (Surgical technique was not described) | Diverticulitis |
| 6 | Thilakawardana et al. [20] | 2017 | 29/M | Acute renal failure | Steroids | NA | Segmental ileal resection | Diverticulitis | |
| 7 | Ramzee et al. [21] | 2020 | 69/M | NA | NA | Ileal diverticulitis | Mesenteric border | Segmental ileal resection Double-barrel ileostomy | NA |
| 8 | Saijo et al. [22] | 2020 | 55/M | NA | NA | Penetration of terminal ileum | Mesenteric border | Ileocecal resection | Diverticulitis |
| No . | Reference . | Year . | Age/ sex . | Past medical history . | Medication . | Preoperative diagnosis . | Perforation site . | Management . | Cause of perforation . |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Miller et al. [16] | 1970 | 49/M | NA | NA | Appendicitis | Mesenteric border | Ileocecal resection | NA |
| 2 | Ackerman [17] | 1974 | Appendectomy Inguinal hernia Heart failure | Various medication | Sigmoid diverticulitis | Mesenteric border | Right hemicolectomy | Diverticulitis | |
| 3 | Roses et al. [5] | 1976 | 30/M | NA | NA | NA | Mesenteric border | Segmental ileal resection | Diverticulitis |
| 4 | Grana et al. [18] | 2009 | 75/M | NA | NA | Penetration of terminal ileum | NA | Right hemicolectomy | Diverticulitis |
| 5 | Kothadia et al. [19] | 2015 | 65/M | Hypertension Angina | NA | Sigmoid diverticulitis | NA | Elective surgery (Surgical technique was not described) | Diverticulitis |
| 6 | Thilakawardana et al. [20] | 2017 | 29/M | Acute renal failure | Steroids | NA | Segmental ileal resection | Diverticulitis | |
| 7 | Ramzee et al. [21] | 2020 | 69/M | NA | NA | Ileal diverticulitis | Mesenteric border | Segmental ileal resection Double-barrel ileostomy | NA |
| 8 | Saijo et al. [22] | 2020 | 55/M | NA | NA | Penetration of terminal ileum | Mesenteric border | Ileocecal resection | Diverticulitis |
M, male; F, female; NA, not available.
The risk of chemotherapy-induced gastrointestinal perforation reportedly increased with angiogenesis inhibitors—such as bevacizumab and ramucirumab—diverticulitis, peptic ulcer, radiation exposure, recent colonoscopy, primary tumor resection, bowel obstruction and multiple surgeries. It often occurred (within the first 6 months) following a few cycles of chemotherapy [22, 23]. Some case reports demonstrated that taxane-induced colitis can lead to colonic perforation requiring surgery. Paclitaxel may induce necrosis of the gastrointestinal mucosa by arresting mitosis of rapidly dividing colonic mucosal cells [24, 25]. In this case, the last dose of bevacizumab was administered more than 6 months before the small bowel perforation. The direct contribution of chemotherapy seems unlikely, and repeated diverticulitis from docetaxel or ramucirumab is suspected of having caused the perforation. The study’s limitations include the inherent limitations of case reports, such as the inability to generalize, prove causality and overinterpretation risk.
The perforation, in this case, may have been caused by repeated diverticulitis triggered by chemotherapy. Despite its low frequency, small bowel diverticula should be considered in patients experiencing unexplained fever and abdominal pain, as diverticulitis can occur in those undergoing chemotherapy. Preventive bowel resection is not required for diverticulitis during chemotherapy, but timely surgical intervention is crucial as diverticulitis in the small intestine has a high mortality rate.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding is available for this study.
AUTHORS’ CONTRIBUTIONS
Study concept and design, acquisition and analysis of data, drafting of the work and surgery: S.K. and S.A. Drafting of the manuscript, critical revision of the manuscript for important intellectual relevance: H.I. and S.I. Revision of the manuscript: H.I., K.S., K.M., S.E., H.M., Y. Yokoyama, Y.N., Y. Yoshioka, T.S., H.S., T.U. Study supervision: S.I.
DATA AVAILABILITY
The data underlying this article will be shared on reasonable request to the corresponding author.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal on request.



