-
PDF
- Split View
-
Views
-
Cite
Cite
Morimoto Shota, Tachibana Toshiya, Iseki Tomoya, Septic retrocalcaneal bursitis in a young soccer player treated with hindfoot endoscopic bursectomy: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 4, April 2023, rjad169, https://doi.org/10.1093/jscr/rjad169
Close - Share Icon Share
Abstract
Septic retrocalcaneal bursitis (RB) is extremely rare with no reports on surgical treatment. Here, we describe a rare case of septic RB in a 14-year-old male soccer player who was treated with hindfoot endoscopic bursectomy. A 14-year-old male soccer player complained of right heel pain without trauma histories when he was playing a soccer. Based on physical examination, radiological findings and laboratory results, we diagnosed the patient with septic RB and started to treat with conservative treatment including a non-weightbearing splint and intravenous antibiotics therapy. However, his symptoms and laboratory results did not improve at 4 days after starting intravenous antibiotics therapy, and so we applied hindfoot endoscopic bursectomy for him. At 4 weeks after the surgery, he could return to the original sport at preinjury level without symptoms and complications. Septic RB in a 14-year-old male soccer player was successfully treated with hindfoot endoscopic bursectomy.
INTRODUCTION
Retrocalcaneal bursitis (RB) is an inflammation of the bursa located between the calcaneus and the Achilles tendon and well known as the common cause of posterior heel pain [1]. The bursitis is commonly caused by overuse involving repetitive impingement of the bursa between the Achilles tendon and the posterosuperior calcaneal prominence [2], frequently occurs in recreational and top runners [3]. On the other hand, septic RB is extremely rare with only one case report [4].
As for treatment of septic bursitis, there is no clear consensus. Conservative treatment involving oral and intravenous antibiotic therapy is generally recommended as an initial treatment [5]. Surgical treatment is applied for cases with significant pointing swelling, cases which are unresponsive to antibiotic therapy alone, chronic cases and recurrent cases [5, 6]. Bursectomy is the most common surgical procedure and is shifting to open procedure to endoscopic procedure in current. Previous literature for septic prepatellar or olecranon bursitis has shown that endoscopic procedure provides satisfactory results with lower complication rates compared to conventional open bursectomy [7–10].
A two-portal hindfoot endoscopic technique was firstly introduced by van Dijk et al. [11]. In recent, this technique has been widely used as a surgical approach for various hindfoot pathologies, because it provides good visualization of the hindfoot structures with lower complication rates compared to traditional open procedure [12]. However, there are no reports on hindfoot endoscopic bursectomy for septic RB.
Here, we describe a rare case of septic RB in a 14-year-old male soccer player who was treated with hindfoot endoscopic bursectomy. Written informed consent was obtained from the patient for publishing this report.
CASE REPORT
A 14-year-old male soccer player who belonged to a junior high school soccer club complained of right heel pain without trauma histories when he was playing a soccer. He had no medical history. He visited a local clinic and was treated with conservative treatment including rest, a non-weightbearing splint and anti-inflammatory medication for 4 days. However, his symptoms got worse, and so he visited our hospital. At the first visit to our hospital, physical examination revealed redness, local heat, swelling and tenderness around the insertion of the Achilles tendon. Also, his right foot was in equinus position, and it was difficult to correct his foot position accurate due to his heel pain (Fig. 1). Plain radiographs showed no abnormal findings (Fig. 2). Magnetic resonance imaging (MRI) demonstrated a low intensity signal on T1-weighted images and a high intensity signal on T2-weighted images in the retrocalcaneal bursa (Fig. 3). Laboratory examination revealed 2.1 mg/dL of C-reactive protein and 7.5 cells × 103/μL of white blood cell count. In addition, ultrasound-guided needle aspiration of the retrocalcaneal bursa resulted in 3 ml of purulent material and in which was positive for methicillin-susceptible Staphylococcus aureus (MSSA). We diagnosed him with septic RB caused by MSSA and started to treat with conservative treatment including a non-weightbearing splint and intravenous antibiotics therapy using cefazolin (6000 mg per day). However, his symptoms and laboratory results did not improve at 4 days after starting intravenous antibiotics therapy, and so we applied hindfoot endoscopic bursectomy for him.

Right foot of the patient was in equinus position, and it was difficult to correct his foot position accurate due to his heel pain.

Plain radiographs of the right ankle showed no abnormal findings in (A) anteroposterior and (B) lateral views.
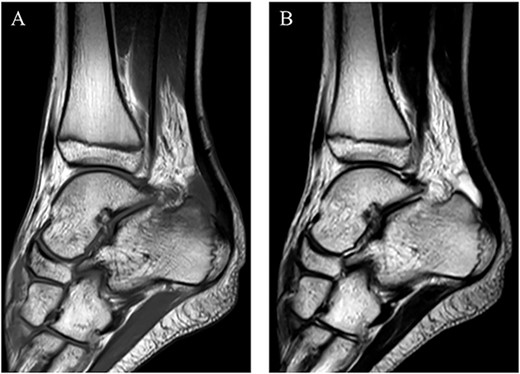
MRI demonstrated a low intensity signal (arrow) on (A) T1-weighted images and a high intensity signal (arrow) on (B) T2-weighted images in the retrocalcaneal bursa.
The surgery was performed under general anesthesia in the prone position using an air tourniquet. Based on the report by van Dijk et al. [11], the posteromedial and posterolateral portals were created. The posterolateral portal was used as a viewing portal, the posteromedial portal as a working portal. First, the anterior aspect of the Achilles tendon was observed using a 4.0-mm-diameter 30° arthroscope. There was hyperemic synovium located between the Achilles tendon and the posterosuperior calcaneal prominence and in which was removed with a 3.5-mm-diameter motorized shaver. After confirming no impingement sign between the Achilles tendon and the posterosuperior calcaneal prominence, the wound was sutured, and so the surgery was concluded (Fig. 4).
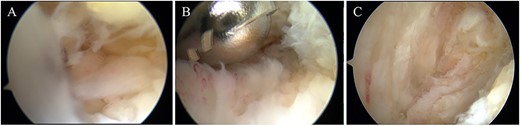
(A) Hyperemic synovium was located between the Achilles tendon and the posterosuperior calcaneal prominence and (B) removed with a 3.5-mm-diameter motorized shaver. (C) After confirming no impingement sign between the Achilles tendon and the posterosuperior calcaneal prominence, the surgery was concluded.
Postoperatively, intravenous antibiotic therapy using cefazolin (6000 mg per day) was continued for 10 days until laboratory results was within normal. A non-weightbearing splint was applied for postoperative 1 week. Active range of motion exercises and partial-weightbearing were started at 1 week postoperatively, and full-weightbearing at 2 weeks postoperatively. At 4 weeks after the surgery, he could return to the original sport at preinjury level without symptoms and complications. In addition, MRI revealed no abnormal signs at 1 year postoperatively (Fig. 5). Two years after the surgery, he remained a competitive soccer player without symptoms and recurrence.

MRI revealed no abnormal signs on short TI inversion recovery images at 1 year postoperatively.
DISCUSSION
Septic bursitis typically occurs through trauma, cellulitis or other skin lesions, and more than half of them are preceded by trauma [13, 14]. It is the common medical condition, superficial bursae such as olecranon and prepatellar bursae are the most affected sites [13, 14]. On the other hand, retrocalcaneal bursae is the deep bursae located between the Achilles tendon and the posterosuperior calcaneal prominence [2], and so septic RB is extremely rare with only one case report [4].
Surgical treatment for septic bursitis generally includes drainage with incision, suction irrigation and bursectomy [5, 6]. Bursectomy is the most common surgical procedure and has traditionally been performed by open approach [7, 8]. However, it has been reported that open bursectomy has a number of potential complications such as wound breakdown and skin necrosis, which requires additional treatment [15]. Recently, there are several reports of endoscopic bursectomy for septic prepatellar or olecranon bursitis [7–10]. These reports have demonstrated that endoscopic bursectomy provides many advantages including low complication rates, shorter hospital stay and a quicker return to work compared to conventional open bursectomy.
In this case, bursectomy was applied because it was unresponsible to antibiotic therapy. Because traditional open bursectomy has a number of potential complications such as wound breakdown and skin necrosis, bursectomy was performed under hindfoot endoscopy. As a result, the patient could return to the original sport at preinjury level without complications at 4 weeks postoperatively.
In conclusion, we reported a rare case of septic RB in a 14-year-old male soccer player who was successfully treated with hindfoot endoscopic bursectomy. This surgical technique may be a useful option in the treatment of septic RB.
CONFLICT OF INTEREST STATEMENT
The author declares that they have no conflict of interest.
FUNDING
No funding.



