-
PDF
- Split View
-
Views
-
Cite
Cite
Saud Alkabbaa, Abdullah M Alsaedan, Alwaleed K Alammar, Pyogenic granuloma of the thumb mimicking squamous cell carcinoma of the nail subunit: case report and review of the literature, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad157, https://doi.org/10.1093/jscr/rjad157
Close - Share Icon Share
ABSTRACT
Pyogenic granuloma (PG) is a benign vascular lesion that usually occurs in the skin or mucous membranes. Multiple theories have been implicated in its aetiology. It can mimic variable malignancies in which histopathological examination plays a vital role. We report a case of PG of the left thumb nail subunit in a 40-year-old gentleman, who presented with left thumb mass after a trauma by a wooden splinter. Incisional biopsy of the lesion could not rule out squamous cell carcinoma. Therefore, full radiological studies were carried out as part of this highly suspicious lesion’s work-up. Excisional biopsy was performed and a full thickness skin graft was harvested from the left distal forearm and applied to cover the defect. Final histopathological examination revealed the diagnosis of PG. The wound subsequently healed well with good functional and aesthetic outcome.
INTRODUCTION
Pyogenic granuloma (PG) or lobular capillary haemangioma is a benign vascular lesion that usually occurs in the skin or mucous membrane presented a single nodule or papule of rapid growth, bleeds easily with only a minimum of trauma [1–5]. It affects both genders and all ages with more tendency towards males and children. Most theories suggest that PG is a hyperplastic, neovascular response to stimulus such as infections, trauma, medications such as retinoids, and hormonal factors [1, 4, 6]. Histological examination revealed capillary proliferation with stromal edema and a mixed inflammatory infiltrate [6, 7]. Diagnosis is usually by history, examination and histopathologic confirmation [1–4, 6]. The main deferential diagnosis for PG is keratoacanthoma, squamous cell carcinoma, basal cell carcinoma, spindle and epithelial cell nevi, melanocytic nevus, Kaposi’s sarcoma, haemangiomas, vascular tumours of intermediate malignancy, amelanotic melanoma and metastatic carcinoma [1–4, 8]. The treatment involves excision of the lesion along with histopathological examination to confirm the diagnosis.
CASE PRESENTATION
A 40-year-old gentleman, otherwise healthy, right-handed, presented with left thumb painless swelling progress rapidly in size over a period of 2 weeks after trauma by a wooden splinter. Initially, he sought medical advice in another facility where he was prescribed topical antibiotic. Nonetheless, the swelling persisted and progress rapidly in size. Of note, the patient mentioned profuse bleeding upon minimal touch, which made him anxious about it and decided to finally seek medical advice in our hospital after 2 weeks from the onset of this swelling. Family, medication and allergic history were all unremarkable.
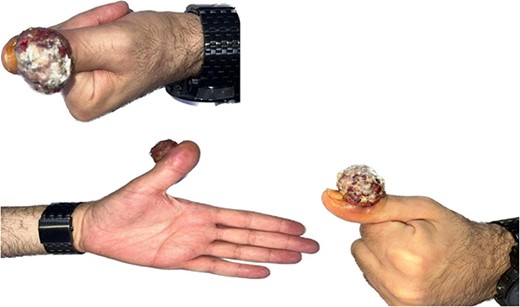
Upon examining the left thumb, an exophytic red, firm, well-circumscribed mass, measuring around 2 × 3 × 4 cm in dimensions, occupied the eponychial fold. The mass had irregular surface with some ulcerations and necrotic tissues (Fig. 1). The mass was not tender, however had the tendency to bleed easily. The thumb interphalangeal joint (IPJ) motions were normal. The left thumb nail plate showed no abnormality apart from the extension of the mass from the eponychial fold to cover almost two-thirds of the nail plate in a frontal view and nearly 50% in a lateral view. There were no other masses or palpable lymph nodes. Examination of the chest and abdomen was unremarkable. All laboratory investigations were within normal values. Hand radiographs revealed a radiopaque soft tissue swelling over the IPJ of the left thumb without bony involvement (Fig. 2). Magnetic resonance imaging of left thumb was conducted and revealed a large hypervascular exophytic lesion of distal thumb, highly suspicious for malignancy, no signs of any bony invasion however the lesion is inseparable from distal fibres of the extensor tendon (Fig. 3). Computed tomography of the chest, abdomen and pelvis was carried out, and revealed multiple enlarged left axillary lymph nodes with no abdominal or pelvic metastasis. Incisional biopsy of the mass reported as extensively ulcerated and necrotic skin, bacterial colonies and tiny foci of capillary proliferation, immunohistochemistry for HHV8 was negative. However, malignancy, namely, squamous cell carcinoma could not be ruled out from this specimen.
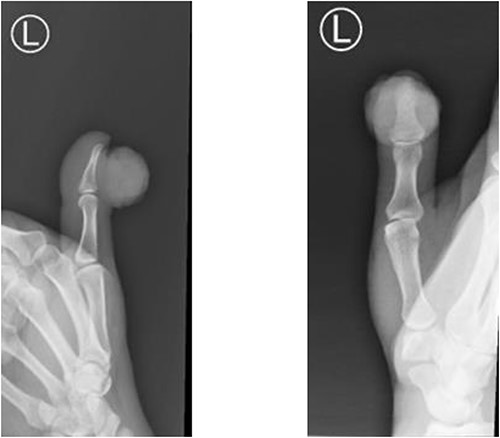
Radiopaque soft tissue swelling over the IPJ of the left thumb without bony involvement.
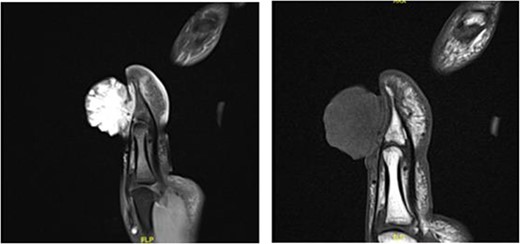
Large hypervascular exophytic lesion of distal thumb, no signs of the bony invasion.
The patient was taken to the theatre under regional anaesthesia. Excisional biopsy with a 4 mm margin including nail plate and nailbed was done, and a full thickness skin graft was harvested from left distal forearm and applied to cover the defect.
Final gross examination revealed a sessile, fragile and haemorrhagic mass measuring 4.7 × 3.7 × 1.5 cm, and subsequent histopathological examination reported as squamous papillomatosis, dermal proliferation of small capillaries, edema, inflammation and ulceration, confirming the diagnosis of PG. On the 5th day postoperatively, the first dressing was changed and showed excellent skin graft take. The patient was referred to occupational therapy thereafter for thumb IPJ range of motion exercises and scar management. Postoperative course was entirely uneventful and the patient has great satisfaction regarding his aesthetic and functional results (Fig. 4). The patient has regular follow-ups to the clinic in order to monitor any signs of possible recurrence, which he does not exhibit.

Three months post-operation, showing a good aesthetic and functional result.
DISCUSSION
PG is a benign vascular lesion that usually occurs in the skin or mucous membranes [1–5]. Most theories suggest that PG is a proliferative response of capillaries to an angiogenic stimulus such as trauma, this theory is similar to our case as this patient suffer from trauma to his thumb [1, 4, 6]. Giblin et al. [9] found that PG had more tendency towards males especially in younger children. However, mucosal lesions occur more in women because of hormonal factors and pregnancy. Histopathological examination is crucial to rule out malignancies. Different management options have been reported, and various treatment outcomes have been described by Giblin et al. [9] in terms of recurrence with surgical excision having the lowest rate of recurrence. No matter what, the definitive management used in treating PG, the risk of recurrence remains uncertain. There are many causes for the recurrence of PG, and incomplete excision is the main cause. In addition, repeated trauma, medications and hormonal oral contraceptives pills can also promote the recurrence [9]. As in our patient, we ensure a full excision of the mass from its base. This is achieved by tracing the base of the mass down to the periosteum and surgically excising it along with 4 mm of safety margin beyond the gross margins of the lesion and with adequate depth in order to ensure complete excision. Histological examination confirmed the completeness of the excision. Post-operative occupational therapy is crucial to prevent stiffness of the IPJ because of scarring from the surgical wound and from unnecessary prolonged immobilization. Our patient developed a decrease in the IPJ flexion a month post-operatively, but almost recovered completely 3 weeks later, with IPJ flexion of 30° and a Kapandji score of 9. In conclusion, tumours involving the nail unit complex should not be taken lightly as many benign lesions could mimic malignancies in their clinical presentations especially in that area and vice versa. Meticulous history taking, thorough examination and work-up, the list of the differential diagnosis can be narrowed and therefore optimal management can take place.
CONFLICT OF INTEREST STATEMENT
No conflict of interest.
FUNDING
None.



