-
PDF
- Split View
-
Views
-
Cite
Cite
Shahana Prakash, Ramses Saavedra, Ryan Lehmann, Mohamad Mokadem, Candy cane syndrome presenting with refractory heartburn 15 years after Roux-en-Y bypass, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad130, https://doi.org/10.1093/jscr/rjad130
Close - Share Icon Share
Abstract
Candy cane syndrome (CCS) is a rare complication of Roux-en-Y gastric bypass (RYGB), in which the afferent jejunal limb is excessively long. Common symptoms include abdominal pain, nausea and vomiting. A 57-year-old female with a history of RYGB 15 years prior to presentation reported 7 months of persistent heartburn refractory to proton pump inhibitors. Upper endoscopy revealed a 9 cm blind, afferent jejunal limb. After the blind limb was resected laparoscopically, her symptoms resolved. Fifteen years is the longest duration reported from time of RYGB to symptom onset of CCS. Furthermore, heartburn is less frequently seen as a presenting complaint of CCS. Clinicians should thus maintain a high index of suspicion for CCS in patients with refractory heartburn and a history of RYGB, regardless of how long ago the RYGB was performed.
INTRODUCTION
The Roux-en-Y gastric bypass (RYGB) is a common bariatric procedure used to induce and maintain weight loss in patients with severe obesity and those with obesity complicated by serious, weight-related comorbidities [1]. Candy cane syndrome (CCS) is a rare complication of this procedure, which occurs when the blind limb of the proximal gastro-jejunal attachment is excessively long (Fig. 1) [2]. Patients with CCS typically present with postprandial epigastric pain, nausea and/or vomiting [2]. The diagnosis of CCS is made based on a combination of history and physical exam, upper endoscopy, computed tomography and/or fluoroscopic imaging [3]. Symptoms usually resolve when the blind, afferent limb is surgically resected [4–6].
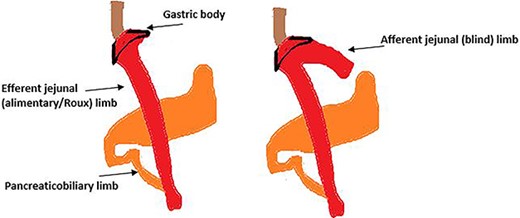
A schematic drawing of normal RYGB anatomy (on the left) and RYGB complicated by CCS (on the right).
Here we describe a case of CCS in a patient who presented 15 years post-RYGB with refractory heartburn, a symptom of CCS which is less commonly seen. Based on current literature available, this is the longest time interval reported from time of gastric bypass to onset of symptoms for this disease process.
CASE REPORT
A 57-year-old female smoker with history of obstructive sleep apnea, severe obesity and history of laparoscopic RYGB 15 years prior to presentation was evaluated in outpatient general medicine clinic after experiencing 7 months of postprandial heartburn. She denied nausea, vomiting, dysphagia, melena, hematochezia or any recent weight changes. Famotidine did not provide relief. Her obesity recurred more than 7 years prior to presentation, and her latest body mass index (BMI) was 42 kg/m2. Her vital signs were normal. Her initial laboratory tests did not reveal leukocytosis or anemia. Her liver panel showed mild elevation of alkaline phosphatase (108 U/L) but was otherwise unremarkable. The patient’s primary care provider switched her regimen from famotidine to daily dosing of omeprazole to treat her symptoms. However, a month later, the patient continued to experience worsening heartburn, along with new-onset nausea. Omeprazole frequency was then increased to twice daily at maximum dose, yet her heartburn and intermittent nausea persisted.
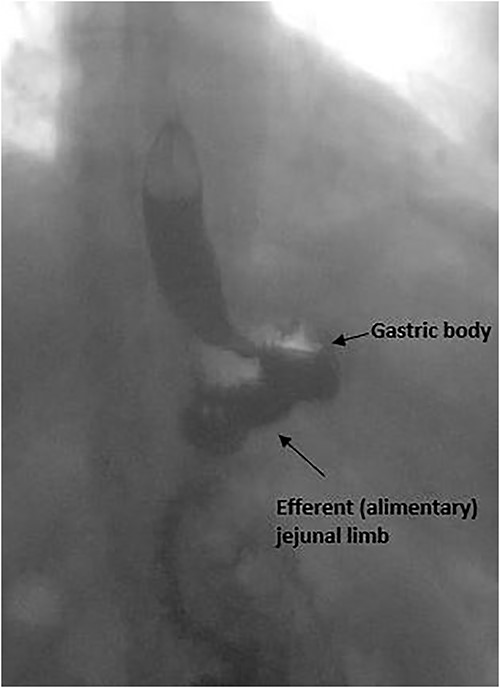
The patient was subsequently referred to gastroenterology clinic for further evaluation. An upper endoscopy was performed, which showed normal gastric bypass anatomy, aside from a blind, afferent jejunal limb measuring 9 cm, raising suspicion for CCS (Fig. 2). The rest of the endoscopic exam was unremarkable. The patient also underwent an upper gastrointestinal fluoroscopy series using barium, which confirmed filling of the long afferent limb first before entering the alimentary or Roux limb (Fig. 3). The patient reported replication of her symptoms with contrast bolus passage during the fluoroscopic exam.
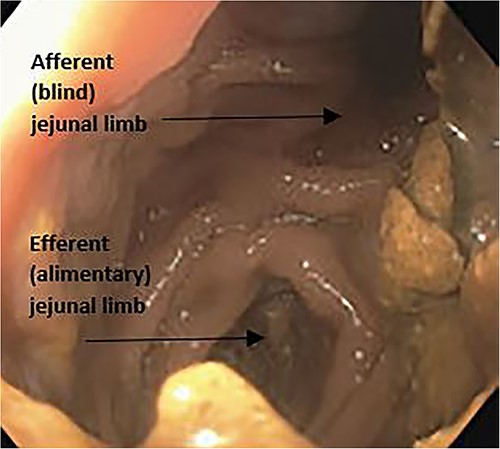
Upper endoscopy image with view from gastric pouch demonstrating both the blind afferent jejunal limb and the alimentary limb.
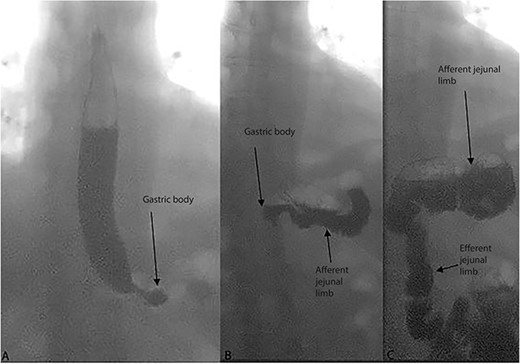
Sequential images of dynamic upper gastrointestinal tract fluoroscopy examination with barium meal in the patient. Opacification is first seen in the esophagus and gastric body (A), followed by the afferent jejunal (blind) limb (B) and last the efferent jejunal (alimentary/Roux) limb (C).
Since the patient’s symptoms persisted, she was referred to bariatric surgery. The patient was offered, and ultimately underwent, excision of the blind limb laparoscopically (seen in Fig. 4).
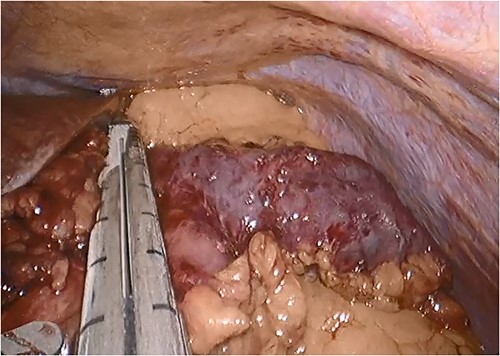
Intraoperative photograph showing the blind, afferent jejunal limb.
At her clinic appointment 4 weeks post-operation, she reported complete resolution of her symptoms, and her BMI had decreased to 37 kg/m2 (from 42 kg/m2 pre-procedure). A follow-up upper gastrointestinal fluoroscopy series confirmed anatomical correction of her CCS anatomy (Fig. 5).
Postoperative images of upper gastrointestinal tract fluoroscopy examination with barium meal, demonstrating anatomy post-resection of the afferent jejunal (blind) limb.
DISCUSSION
CCS is a result of an excessively long afferent gastro-jejunal limb after a Roux-en-Y bariatric surgery (Fig. 2). The diagnosis of CCS can be challenging, as symptoms overlap with several other conditions, including bacterial overgrowth, functional gastrointestinal motility disorders and complications of gastric bypass, such as strictures or ulcers [4, 7, 8].
The pathophysiology of CCS is party mechanical, in that the redundant Roux tip serves as a blind pouch for food to accumulate, which, in turn, increases luminal pressure and causes dilatation, especially with overeating [4]. Furthermore, poor drainage, consequent bacterial overgrowth and intussusception of the afferent limb into the stomach may be other factors at play [6, 9, 10]. The largest (n = 47) retrospective study found that the most common symptoms associated with CCS were abdominal pain (100% of patients), nausea (66% of patients) and vomiting (35% of patients); the least common symptom was that of reflux or heartburn, which 17% of patients reported on presentation [6]. There were no patients in this study who presented with isolated heartburn. In our case, the patient was unique in that she presented with only heartburn for 7 months, prior to the development of nausea. Literature review only revealed one CCS case that was somewhat similar, in a 40-year-old female, who, 8 years after bypass, presented with intractable heartburn and nausea; however, even in this case, nausea and heartburn occurred simultaneously (i.e. heartburn did not precede nausea) [11]. While the shortest reported time interval from gastric bypass to symptom onset of CCS is 3 weeks, the longest time reported is 11 years [4]. In our patient’s case, the time interval was 15 years, making it the longest time interval reported between RYGB and symptom onset of CCS. This feature in combination with her atypical symptom of heartburn at presentation makes her case unique.
The clinical diagnosis of CCS is made based on a combination of history and physical exam, endoscopy, computed tomographic and/or dynamic fluoroscopy [3]. Treatment of CCS is resection of the redundant limb. The laparoscopic surgical approach has been shown to be safe and feasible [4]. Following resection of the candy cane, some extent of weight loss often follows, as the candy cane itself is otherwise a reservoir for excess food [4].
To avoid CCS, bariatric surgeons should avoid creating a blind loop or limb at the gastrojejunostomy. This patient case is notable in that the patient developed reflux symptoms nearly 15 years after her initial bypass, which is the longest reported time interval from initial bypass to symptom onset for CCS. While abdominal pain, nausea and vomiting are the most frequent symptoms patients experience with CCS, heartburn is another less common presenting complaint that can occur with this condition. Thus, clinicians should maintain a high index of suspicion for CCS in patients with refractory, new-onset heartburn, regardless of when the RYGB was performed. This will ensure timely intervention if needed.
CONFLICT OF INTEREST STATEMENT
All authors declare no conflict of interest related to the content of this manuscript.
FUNDING
This work was supported by Merit grants from the US Department of Veterans Affairs (#I01 BX004774 and #I01 BX005173) awarded to M.M. The contents do not represent the views of the US Department of Veterans Affairs or the US Government.
DATA AVAILABILITY
All data related to the content of this case report are present within the body of the manuscript.
AUTHORS’ CONTRIBUTIONS
S.P. and M.M. conceived, designed and drafted the manuscript. R.S., R.L. and M.M. contributed to the pathological diagnosis and management decision in caring for the patient. All authors have read and agreed to the published version of the manuscript.



