-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie Chan, Ursula Kemp, Sheen C Peeceeyen, A rare care of Lomentospora prolificans sternal wound infection post aortic valve replacement—an approach to surgical management, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad123, https://doi.org/10.1093/jscr/rjad123
Close - Share Icon Share
Abstract
A 77-year-old woman underwent surgical aortic valve replacement via hemisternotomy. Her post-operative course was unremarkable. Owing to travel and contact restrictions during the COVID pandemic, she was unable to attend routine follow up. She continued review with her local medical officer in regional New South Wales. Post 6 months following her index surgery, she was referred to the Infectious Disease Clinic of her local hospital with a non-healing lesion at the base of her hemi-sternotomy wound. Computed tomography revealed a deep sternal wound infection which extended deep to bone. She was admitted to hospital for treatment. The primary pathogen identified was Lomentospora prolificans—a dangerous fungus that affects immunosuppressed patients. Strong antifungal and adjunctive antibiotics did not contribute much to clearance of infection. Radical surgical debridement was required to obtain clean tissue margins.
INTRODUCTION
Median sternotomy complications occur in in 0.5–5% of patients, with the incidence in most centers being between 1 and 2%. The majority of patients have monomicrobial infections. The vast majority of these infections are caused by bacteria. Rarely, post-operative mediastinitis is due to unusual organisms such as fungi [1].
CASE REPORT
Ms GL, a 77-year old woman, underwent surgical aortic valve replacement in May 2021. She was discharged routinely on post-operative Day 7. Her past medical history included emphysema (due to long-term smoking).
She did not attend her surgical follow up appointment, choosing to participate in telehealth due to the COVID pandemic. She was seen in person by her GP, and her cardiologist, who both noted some redness relating to her sternal wound, and a small soft tissue eruption at the inferior aspect (Fig. 1). Ongoing non-specific chest pain was dismissed as post-operative. She was prescribed several courses of oral antibiotics (amoxycillin/augmentin DF).

The lesion continued to grow. Blood investigations demonstrated a slightly elevated CRP (~120) and normal white cell count. Several months later, a ‘satellite’ nodule appeared inferiorly (around the xiphoid process) (Fig. 1). Contact was subsequently made with her surgeon, who organised for a in-person review. The patient was admitted directly to hospital for urgent treatment in November 2021 (Fig. 2).
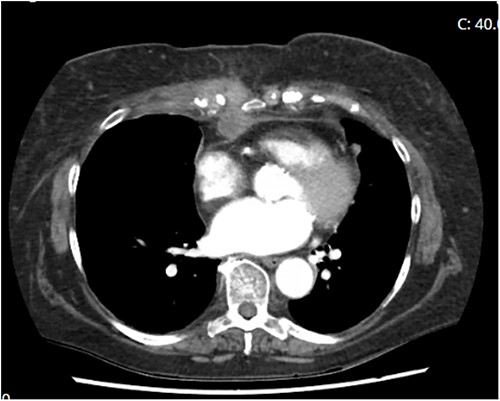
Computed tomography demonstrating penetrance of infection deep to sternum.
Ms GL was diagnosed with a deep sternal wound infection. The most common infective agent implicated in DSWI is Staphylococcus (followed by Enterococcus). This atypical sternal wound infection was positive for fungal growth, specifically Lomentospora prolificans—a dangerous and resistant pathogen that affects immunosuppressed patients [2]. This was treated with a combination of voriconazole and miltofosine under the instruction of infectious disease physicians [3].
Ancillary polymicrobial growth (including Corynebacterium tuberculostearicum, Staphylococcus epidemidis, Staphylococcus capitus and vancomycin-resistant Enterococcus faecium) was successfully treated with meropenem.
Regardless of the pathogen, sternal wound breakdown requires aggressive surgical management. Particularly in the case of fungal pathogens, the mainstay of treatment is removal of infected tissue, removal of any hardware (or other sternal closure devices/foreign material), and adjunctive antimicrobial therapy.
Although antimicrobials play a large role in the eradication of bacterial pathogens, antifungal therapies are not as contributory to the eradication of fungal infections [4]. Aggressive debridement (including sternectomy and excision of costal cartilages) was performed with the assistance of plastic surgery teams (Fig. 3). In early December 2021—after 10 surgical debridement surgeries—clean margins and negative cultures were obtained. The wound bed was deemed suitable for reconstructive surgery with omental flap and skin graft.
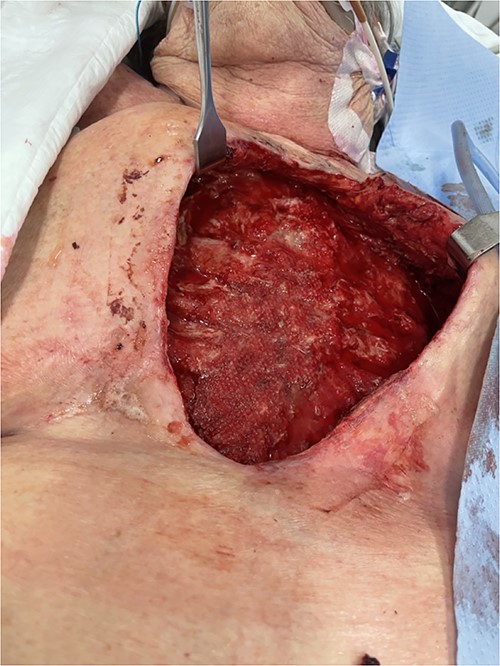
Sternectomy and costochondrectomy required for pathogenic clearance.
Sadly, the toxicity of the anti-fungal treatments resulted in hepatic and renal failure, and the duration of time required to obtain fungal clearance had left Ms GL deconditioned, with hepatic and renal failure. She passed away before reconstruction was undertaken.
DISCUSSION
Fungal sternal wound infections need early and aggressive surgical management as the mainstay of treatment. Antifungal therapies can only provide adjunctive therapy. Where necessary, aggressive (even radical) excision should be undertaken early. This may minimise the duration of therapy and hepatotoxic (and other systemic) effects of concurrent medical treatments.
Moreover, this case serves as a timely reminder that problematic surgical wounds should be reviewed in person by the operating surgeon—general practitioners are not experienced in the assessment of atypical wounds. Telehealth should only be used in clearly ‘routine’ follow-up.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- antibiotics
- computed tomography
- aortic valve replacement
- antifungal agents
- debridement
- drug clearance
- mycoses
- follow-up
- immunocompromised host
- scedosporium
- sternum
- surgical procedures, operative
- infections
- fungus
- plastic surgery specialty
- plastic surgery procedures
- pathogenic organism
- sternum wound infections
- pandemics
- telehealth
- postoperative deep sternal wound infections



