-
PDF
- Split View
-
Views
-
Cite
Cite
Akio Sakamoto, Takashi Noguchi, Shuichi Matsuda, Combined latissimus dorsi and scapular flaps for reconstruction of a large defect after a shoulder sarcoma resection, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad121, https://doi.org/10.1093/jscr/rjad121
Close - Share Icon Share
Abstract
Reconstruction with a pedicled latissimus dorsi flap is used for a large defect after resection of soft tissue sarcoma of the shoulder. Primary donor site closure is sometimes difficult and a skin graft is necessary, possibly delaying postoperative chemotherapy. Combined latissimus dorsi and scapular flaps are used for free flaps in head and neck reconstruction. Myxofibrosarcoma resection in the shoulder of a 76-year-old man resulted in a 16 cm diameter skin resection. The defect was reconstructed with a scapular flap (width = 5 cm) for the distal defect and a pedicled latissimus dorsi muscle flap (flap size, 10 × 7 cm) for the proximal defect. Primary closure of the donor site in the latissimus dorsi flap was easy. By adding a scapular flap to the latissimus dorsi flap, the latissimus dorsi flap area can be reduced, making it easy for primary suture and contributing to less invasive surgery.
INTRODUCTION
Soft tissue sarcomas are neoplasms that can occur in superficial parts of the body. Wide resection of the sarcoma and the surrounding normal tissue is necessary. Flap techniques are widely used to repair soft tissue defects. Myxofibrosarcomas occur in the subcutaneous tissues of superficial soft tissues [1]. The recurrence rate of superficial myxofibrosarcomas is related to the characteristics of the resection. The recurrence rates of wide, marginal and incomplete surgical margins have been reported to be 25, 50 and 67%, respectively [1]. Therefore, to reduce possible recurrence rates, adequate wide resection is necessary.
A latissimus dorsi flap is widely used for reconstruction after sarcoma resection. A primary suture is possible with a width < 8–9 cm. With a defect >12 cm in width, however, the primary suture is difficult [2]. A skin graft for the donor site is necessary, and the graft may require a longer healing time and can result in a delay of postoperative adjuvant therapy for sarcoma treatment. Latissimus dorsi muscle and scapular (bone) flaps are used as composite flaps for craniofacial reconstruction [3]. In this report, combination pedicled latissimus dorsi and pedicled scapular flaps were used for reconstruction after resection of superficial sarcomas in the shoulder. The usefulness of the combination is shown by a comparison with a similar defect reconstructed with latissimus dorsi flap alone.
CASE REPORTS
Case 1
A 76-year-old man had an enlarging soft tissue mass in the right shoulder for >1 month. Resection of the tumor was attempted under the diagnosis of a cystic lesion, but the procedure was stopped after the skin incision at the initial hospital. The patient was referred to our institute with a working diagnosis of a solid malignant tumor. On physical examination, a protuberant, elastic, hard mass was palpable without tenderness. Magnetic resonance imaging (MRI) showed a subcutaneous tumor with a maximum diameter of 6 cm. The tumor had a homogenous low-signal intensity on the T1-weighted image and a high-signal intensity on the T2-weighted image (Fig. 1). A histologic examination of a needle biopsy specimen revealed a myxofibrosarcoma.
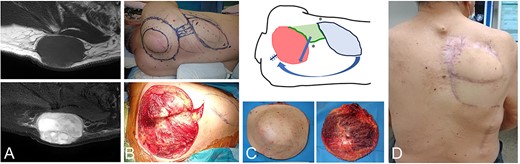
A 76-year-old male with a fibrosarcoma in the right posterior shoulder. MRI shows a subcutaneous tumor with a low-signal intensity on the T1-weighted image (A-top) and a high-signal intensity on a T2-weighted fat-suppressed image (A-bottom). After resection of the tumor with the surrounding tissue (B), the schematic reconstruction design is shown (C-top). The resected tumor was covered by normal skin and muscle tissue (C-bottom). The light green area is the scapular flap and the light blue area is the latissimus dorsi. Arrows show the direction of flap translocation. Asterisks (*) are sutured points. Postoperative view 2 years after reconstruction (D).
Resection was performed under general anesthesia. The patient was placed in a lateral position. The tumor was resected with >3 cm margins of normal tissue from the abnormal MRI signal intensity, resulting in a resected skin that was round-shaped and 16 cm in diameter. The circumflex scapular artery was confirmed to be intact. The size of the pedicled scapular flap was 5 cm wide and was reconstructed at the distal part of the defect. Then, the latissimus dorsi muscle with its skin paddle was elevated, in which the full width of the 10 × 7 cm latissimus dorsi muscle and skin flap was harvested. The width in the donor site was 7 cm and closed easily. Two years postoperatively, no recurrence was detected and there was no disability in shoulder movement.
Case 2
An 87-year-old man had a right shoulder mass over several months. The physical examination revealed an elastic, hard mass on the right shoulder that was 6 cm in diameter. An MRI showed a tumor with a homogenous low-signal intensity on the T1-weighted image and a heterogenous low-high signal intensity on the T2-weighted image (Fig. 2). The size, including the abnormal signal intensity, was 9 cm. The tumor was attached to the scapular spine. A histologic examination of a needle biopsy specimen revealed a leiomyosarcoma. The surgical resection with 3-cm margins from the abnormal MRI signal intensity was performed. The resection included the underlying muscle and the scapular spine. The resected skin size was round-shaped and 15 cm in diameter. The latissimus dorsi muscle with its skin paddle was elevated, in which the full width of the 10 × 17 cm latissimus dorsi muscle and skin flap sized was harvested. The 10-cm donor site closed primarily, but the tension was tight. The postoperative course was uneventful.
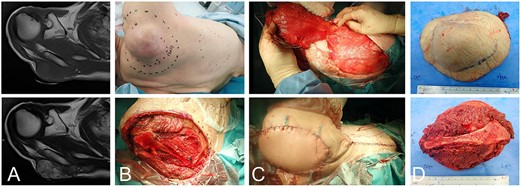
An 86-year-old male with a leiomyosarcoma in the right posterior shoulder. The subcutaneous tumor with a low-signal intensity on the T1-weighted image (A-top) and a heterogenous low-high signal intensity on the T2-weighted image (A-bottom). The surgical margin is designed (B-top) and resected with the underlying scapular spine (B-bottom). The latissimus dorsi is elevated (C-top). The primary suture is completed, but tight. Note that the skin at the possible scapular flap is loose (C-bottom). The resected sample is covered with normal tissue, including the scapular spine (D).
DISCUSSION
The prolonged time until complete healing of a skin graft at the donor site can be a disadvantage of a latissimus dorsi flap in the treatment of a soft tissue sarcoma [4]. Therefore, primary closure of the donor site is recommended. In the current case, the width of the donor site in the latissimus dorsi flap combined with a scapular flap in the myxofibrosarcoma case was 7 cm, whereas the latissimus dorsi flap in the leiomyosarcoma case was 10 cm. The primary closure was possible in both cases; the former case was straightforward, but the latter case was tight. It has been reported that an approximate 10 cm border between the primary suture and skin graft is optimal [2].
Latissimus dorsi and scapular flaps have the same vascular pedicle (the thoracodorsal artery). Therefore, a combination of latissimus dorsi and scapular flaps are used for free flaps in craniofacial reconstruction as composite free flaps [3]. For the treatment of a soft tissue sarcoma, combined latissimus dorsi and paddle scapular flaps for a large defect after soft tissue sarcoma resection is recommended [5]. The transverse cutaneous branch from the thoracodorsal artery has a scapular cutaneous branch (scapular flap) in the medial direction or a parascapular cutaneous branch (parascapular flap) in the descending direction in scapular flaps [6]. In using a parascapular cutaneous paddle, the flap can be made at the distal of the scapula. Therefore, the current combination of latissimus dorsi and scapular flaps or a parascapular flap can cover a defect involving the entire scapular region. In our two cases of flap reconstructions, no dysfunction of the shoulder was noticed with respect to activities of daily living. In a previous report involving latissimus dorsi reconstruction, shoulder dysfunction associated with the latissimus dorsi flap has been reported to recover over the first year [7].
In summary, a combination of latissimus dorsi and scapular flaps can reduce the area of the donor of the latissimus dorsi flap, which makes it easy for primary suture and contributes to less invasive surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DATA AVAILABILITY
There are no new data associated with this article.
References
- chemotherapy regimen
- reconstructive surgical procedures
- sarcoma
- skin transplantation
- surgical procedures, operative
- sutures
- shoulder region
- skin
- surgery specialty
- free flap
- head and neck reconstruction
- latissimus dorsi muscle
- soft tissue resection
- myxofibrosarcoma of skin
- latissimus dorsi flap
- donor site
- scapular flap



