-
PDF
- Split View
-
Views
-
Cite
Cite
Elissa Jie Zhang, James Wei Tatt Toh, Severe constipation causing ischaemic stercoral perforation of sigmoid colon, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad105, https://doi.org/10.1093/jscr/rjad105
Close - Share Icon Share
Abstract
Stercoral perforation is a rare but life-threatening condition that is increasingly being recognised as a sequelae of severe constipation. We present the case of a 45-year-old female who presented with stercoral perforation secondary to severe constipation related to adjuvant chemotherapy for colorectal cancer on a background of long-term antipsychotic medications. Chemotherapy-induced neutropaenia posed an additional treatment consideration in the management of sepsis associated with stercoral perforation. This case demonstrated that the morbidity and mortality from constipation especially in at risk patients cannot be underestimated.
INTRODUCTION
Stercoral perforation is a rare but life-threatening condition that is increasingly being recognised as a real entity associated with severe constipation. Systematic reviews thus far have identified approximately two hundred patients diagnosed with stercoral perforation, although it is likely that it has been significantly under-reported [1, 2]. Although the mechanism is not fully understood, it is thought that impacted faecalomas may cause local pressure with subsequent ischaemia and necrosis of the colonic wall, leading to a stercoral ulcer or perforation [3]. The rectosigmoid colon is most commonly affected. Perforations are typically located on the antimesenteric edge [4]. The distal colon is most commonly affected due to inspissated faecalomas [5]. Risk factors associated with stercoral perforation include chronic constipation, increasing age, smoking, chronic opioid use/medications associated with constipation such as anti-psychotic drugs including clozapine [6, 7]. Diagnosis is confirmed by CT imaging of the abdomen and pelvis usually necessitating a laparotomy. The risk of mortality increases with the degree of faeculent peritonitis, septic shock, clinical deterioration as well as in patients with immunocompromised states and significant comorbidities [8].
CASE REPORT
In this case, we present Ms IW, a 45 year old female who had an acute emergency presentation to a tertiary referral hospital with twelve hours of severe lower abdominal and a single episode of bright red per rectal bleeding. While in the emergency department, she rapidly deteriorated with worsening pain, tachycardia and high-grade fevers. Several months prior to emergency presentation, Ms IW was diagnosed with right-sided colon cancer with pelvic side wall lymph node metastases for which she had successful surgery with curative intent with R0 resection. She had just completed a short course of radiotherapy to her pelvis and had commenced adjuvant FOLFOX chemotherapy 1 week prior to her emergency presentation. She had schizophrenia for which she was on long-term Clozapine 300 mg daily. This medication can be associated with severe constipation which the patient denied experiencing prior to the commencement of chemotherapy. She experienced significant chemotherapy adverse effects of nausea, abdominal discomfort and constipation.
On CT of her abdomen and pelvis, there was a large volume of pneumoperitoneum and a massive sigmoid faecaloma suggestive of stercoral perforation associated with ischaemic changes (Fig. 1). She underwent emergency laparotomy, which identified a grossly dilated and redundant sigmoid colon impacted with a large, inspissated faecaloma >15 cm in diameter (see Figs 2 and 3). The perforation was identified in the mid to distal sigmoid colon with evidence of necrosis of the wall. A Hartmann’s procedure and extensive washout was performed. Post-operatively, the patient required vasopressor support for septic shock in intensive care, as well as granulocyte colony stimulating factor (G-CSF) to help in the management of her febrile neutropaenia. Her Clozapine was suspended for several days due to her neutropenia. She was given G-CSF to improve her neutropenia to improve her chances of survival as it known that immunocompromised patients with sepsis have worse prognosis [9]. Fortunately, the patient recovered well post-operatively and was discharged to rehabilitation on day 10.
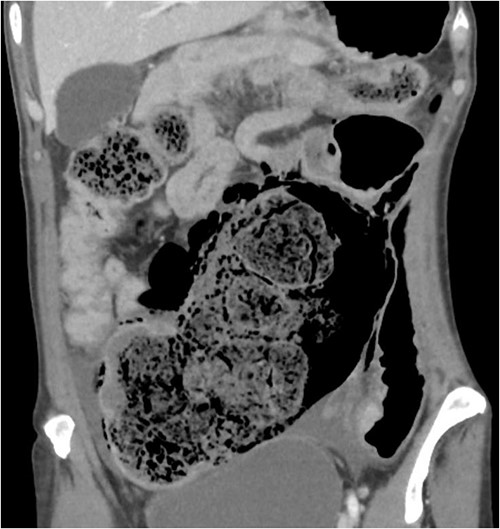
CT abdomen pelvis demonstrating inspissated with faecaloma with pneumatosis and adjacent free gas.
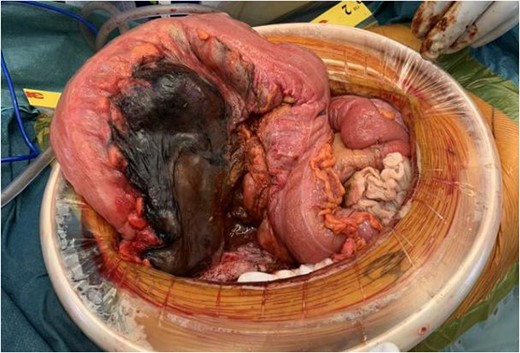
Intraoperative findings of ischaemic stercoral perforation of the sigmoid colon.

Resected specimen demonstrating ischaemic necrosis and faecaloma through large stercoral perforation.
Histopathology confirmed the presence of a full thickness perforation approximately 50 mm in length, with surrounding ischaemic necrosis of the mucosa and a massive faecaloma, confirming the diagnosis of stercoral perforation associated with ischaemia. Although there have been limited case reports of stercoral perforation described in schizophrenic patients requiring Clozapine and other antipsychotics that have a constipating effect [6, 10], Ms IW had been on long-term Clozapine and her stercoral perforation was believed to be associated with her comorbidities and adjuvant chemotherapy, not just associated with Clozapine.
DISCUSSION
Stercoral perforation is a clinical entity that is widely debated with many arguing that the mechanism of perforation is associated with other conditions such as diverticulitis, traumatic injury, inflammatory bowel disease or other diseases that cause a pre-existing weakness in the bowel wall rather than from constipation.
Maurer et al. proposed four criteria for the diagnosis of stercoral perforation constituting of (i) an antimesenteric colon perforation greater than 1 cm in diameter; (ii) stool in the colon protruding through the perforation site; (iii) evidence of pressure ulceration and acute inflammation on microscopy of the perforated site; and (iv) absence of other causes of perforation such as trauma, diverticulitis, neoplasm or adhesions [4].
In this case, the patient met all four criteria. Furthermore, Fig. 1 clearly shows that the pressure effect from an impacted inspissated faecaloma can cause necrosis of the bowel wall in the absence of diverticulitis, neoplastic lesion and adhesions as the adjacent bowel was healthy without other disease processes. This case report supports that stercoral perforation from chronic constipation is a real entity. The old adage that constipation can kill is not a myth.
ACKNOWLEDGEMENT
We would like to acknowledge the patient for providing informed consent and allowing the case to be reported and published.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
DECLARATIONS
Consent was obtained from patient to publish this clinical case and related images.
DATA AVAILABILITY
The authors may be contacted regarding data availability and clarification.



