-
PDF
- Split View
-
Views
-
Cite
Cite
Nawaf R Alsubaie, Mohammed A Ibrahim, Mahmoud A Nassar, Mohammad I Alsalama, Appendicular mucinous cystadenoma: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad097, https://doi.org/10.1093/jscr/rjad097
Close - Share Icon Share
Abstract
Mucinous cystadenoma of the appendix is a rare condition characterized by abnormal mucus accumulation in the appendiceal. Laparoscopic appendectomy is a common approach worldwide and can be used in the management of mucinous cystadenoma with lower postoperative complication rates. A 30-year-old female had sharp pain localized to the right abdomen for 2 days. It was aggravated by movement and associated with nausea and vomiting. Laboratory findings were normal, but the abdominal computerized tomography scan demonstrated a cystic tumor in the right abdomen dorsal to the cecum and the ascending colon. Diagnostic laparoscopy showed a large cystic mass well-circumscribed encapsulated involving the appendix in the lower right abdomen. After demonstrating pathologic examination, the final diagnosis was mucinous cystadenoma of the appendix. Management of the appendicular mucinous cystadenoma can be successfully achieved through atraumatic laparoscopic excision of the tumor, it is safe, feasible and has a short postoperative recovery period.
INTRODUCTION
Mucinous cystadenoma of the appendix is the most common form of appendiceal mucocele (AM); yet its clinical, radiological and gross examination are non-characteristic [1].
Preoperative diagnosis of appendiceal mucinous cystadenoma is usually difficult as most patients are asymptomatic. Lesions are incidentally discovered during exploratory surgeries, investigations for another condition or through a postoperative histopathological examination [2].
Management of AM requires surgery for complete and cautious excise of the mucocele. Mass rupture during surgery may lead to pseudomyxoma peritonei (PMP), which is a rare condition that usually arises as a complication of appendiceal neoplasms [3–6].
The use of laparoscopic appendectomy in mucinous cystadenoma is questionable as it requires a special atraumatic process to avoid the spread of mucin into the peritoneal cavity. Recently, some studies have supported laparoscopy safety and feasibility [7, 8].
CASE REPORT
A 30-year-old female presented to the emergency department due to severe abdominal pain for 2 days. The pain was constant and sharp, localized to the lower abdomen more in the right iliac fossa (RIF). It was aggravated by movement, associated with vomiting, a history of frequent urination, and it was recurrent for the last month.
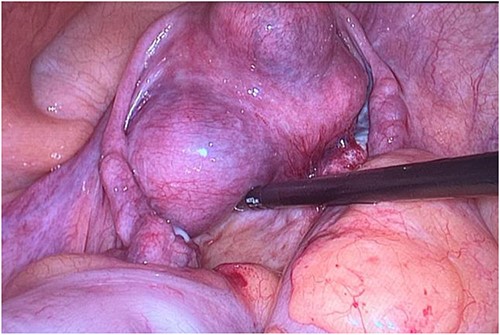
She had a previously diagnosed uterine fibroid as shown in Fig. 3. Otherwise, she had no significant medical or surgical history.
Abdominal examination revealed a local rebound tenderness in the RIF, but no mass was palpable. Blood tests and urine analysis and culture were normal.
Abdominal ultrasound and computerized tomography (CT) scan demonstrated a cystic tumor, 13 × 3 cm, in the right abdomen dorsal to the cecum and the ascending colon. No lymph node swelling or fluid collection was illustrated in Fig. 1.

Pre-operative Computed tomography scan showing appendix mucocele.
Laparoscopic surgery was performed due to suspected appendicitis. With the patient in the supine position, a closed pneumoperitoneum was created using a Veress needle in Palmer’s point. The scope was inserted through a supra-umbilical incision using a 12-mm Visi-port trocar. After inspection, 12- and 5-mm assistant trocars were inserted.
Diagnostic laparoscopy showed a large cystic mass well-circumscribed encapsulated involving the appendix without its base as shown in Fig. 2. No invasion was observed, no free fluid in the peritoneal cavity, and the liver and the omentum were clear of mucoid fluid and nodules.
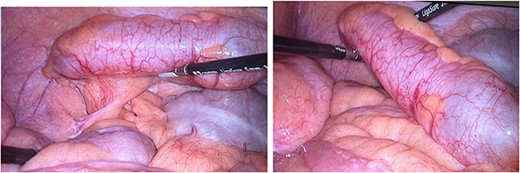
Operative photograph showing large mucinous cystadenoma of the appendix.
Then appendectomy was performed, with the patient in the reverse Trendelenburg position, using an endoscopic bag with no peritoneal cavity spillage, and minimal manipulation with (non-traumatic) graspers.
The patient had an uneventful postoperative recovery. Postoperative pain was minimal, and the patient was ambulatory the next day. She started clear liquid on the first postoperative day and was discharged home on the third postoperative day (Fig. 3).
A gross pathologic examination demonstrated a 10 × 3-cm cystic structure. Microscopic examination revealed a cellular atypical epithelium. The absence of malignant cells was confirmed, no mucin dissects or invade the appendicular wall, no mucin on the serosal surface or in the adipose tissue. Hence, the tumor, illustrated in Fig. 4, was diagnosed as mucinous cystadenoma of the appendix. Ten-month post-operation, a follow-up CT scan revealed no abnormal focal PMP at the peri-cecal region.

DISCUSSION
Mucinous cystadenoma is the most common benign appendiceal tumor [9]. The condition can be asymptomatic or may present with abdominal pain; thus, the preoperative diagnosis is difficult. In the present case, our patient had a two-day history of pain in her RIF. The gold standard diagnostic is non-invasive imaging modalities, ultrasound and CT [10, 11].
Management of mucinous cystadenoma using laparoscopy requires careful and atraumatic technique to minimize the risk of rupture and peritoneal seeding. However, several articles reported that laparoscopic approaches have been used successfully for the resection of mucinous neoplasms [12–14]. During the surgery, the entire abdominal cavity should be checked for mucinous fluids accumulation [11, 15].
Previous multiple laparoscopic intervention cases have shown no radiographic evidence of recurrence or PMP. This proves the feasibility and safety of a laparoscopic approach for preoperative diagnosis and management of mucocele of the appendix [10].
In summary, the clinical benefit of laparoscopic resection of the mucocele is that it is a minimally invasive procedure with slight postoperative complications. Additionally, studies have shown no evidence of rupture or dissemination. Appendicular mucinous cystadenoma should be included in the differential diagnosis when ultrasonography or CT detects a cystic mass in the lower right abdomen.
CONSENT
Written informed consent was obtained from the patient for publication of this Case report and any accompanying images.
CONFLICT OF INTEREST STATEMENT
No conflict of interest was declared by the authors.
FUNDING
This study has received no financial support.



