-
PDF
- Split View
-
Views
-
Cite
Cite
Marlie H Fisher, Jack F C Woods, Edmund K Bartlett, Jonas A Nelson, A rare case of rhabdomyosarcoma identified in a VRAM flap after lower extremity reconstruction, Journal of Surgical Case Reports, Volume 2023, Issue 3, March 2023, rjad083, https://doi.org/10.1093/jscr/rjad083
Close - Share Icon Share
Abstract
Spindle cell sclerosing rhabdomyosarcoma (sc-RMS) is an extremely rare soft tissue tumor. We report an unusual case of sc-RMS in a 36-year-old patient whose tumor arose in a rectus abdominis muscle free flap that had been used for lower extremity reconstruction 18 years previously. After surgical excision of the tumor and immediate reconstruction, the patient has remained in remission and has full function of his lower extremity six months after diagnosis and treatment.
INTRODUCTION
Rhabdomyosarcoma (RMS) is a common soft tissue malignancy of children, but is exceedingly rare in adults [1]. The spindle cell variant of embryonal rhabdomyosarcoma has been recently reclassified to distinguish it from the classical histologic subtypes of embryonal, alveolar and pleomorphic, as it has distinct molecular, morphologic and clinical behavior [2]. Emerging molecular data reveals these mutations to harbor recurrent fusions and mutations in MYOD1 [3]. While only isolated reports have been described, sc-RMS is more common in the head and neck region, followed by the retroperitoneum, thigh, leg and subscapular areas [4]. In the adult population, sc-RMS does not have the prognostic advantage that it does in pediatric populations and tends to recur [5, 6].
CASE REPORT
A 36-year-old male was referred to our center with a newly diagnosed spindle cell sclerosing rhabdomyosarcoma of the left lower extremity. The patient had a history of a left lower extremity crush injury with an iron beam in 2004. This injury resulted in multiple surgeries and debridement procedures with limb shortening and reconstruction with a free rectus abdominis muscle flap and a skin graft to the medial aspect of the middle third of the leg. He had subsequent bone transport surgery to lengthen the limb, resulting in good limb and ankle function.
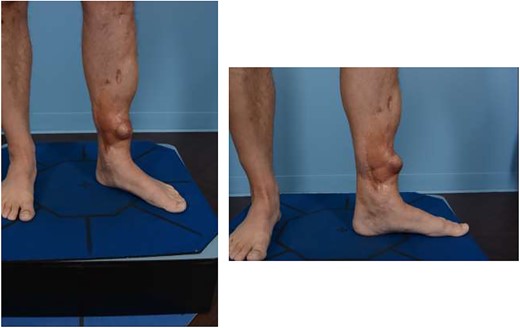
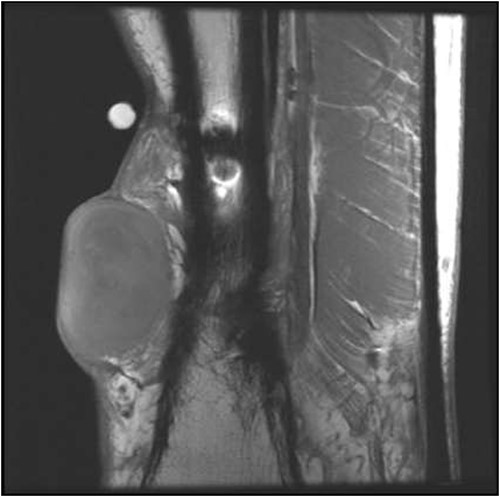
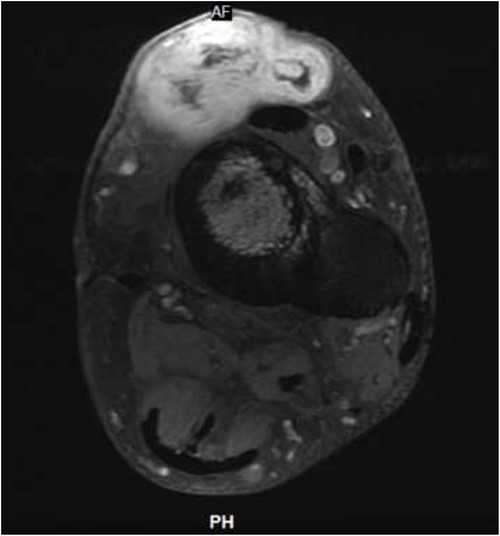
He presented upon noticing a lump overlying the rectus flap. On exam, the left lower extremity had multiple incisions with well-healed scars and a protruding lesion at the distal aspect of his previous incision, which was non-tender to palpation (Fig. 1). MRI of the lower extremity revealed a soft tissue mass in the anterior compartment of the left lower extremity (Figs 2 and 3). Biopsy of the lesion demonstrated RMS and molecular diagnostics revealed missense mutations in MYOD1 (p.L122R) and DOT1L (p.G1441R). Tumor cells were microsatellite stable. The copy number profile is suggestive of broad copy number gain of chromosome 5p. The patient was discussed at the local tumor board and was treated with D9803 chemo protocol (vincristine-based), receiving 4 cycles before proceeding to operative management.
For resection, 2-cm margins were planned circumferentially around the lesion and the periosteum of the tibia underlying the mass was stripped and kept as a deep margin. Only the portion of the previous rectus muscle flap that fell within the 2-cm margins was excised. Pre-operatively, CT angiography demonstrated a patent vascular pedicle to the previous rectus abdominis flap, which had been anastomosed to the posterior tibial vessels. The pedicle was identified intra-operatively at its former anastomosis and followed into the rectus flap to a point where it was clear from scar tissue. Pencil Doppler signals were present in the artery, and venae comitans and inflow to the artery were confirmed under direct vision. An anterolateral thigh (ALT) fasciocutaneous free flap was used to reconstruct the defect, anastomosing end-to-end onto the deep inferior epigastric artery and one venae comitans. In order to ensure adequate venous outflow, a second venae comitans from the ALT was anastomosed to the great saphenous vein.
Surgical pathology confirmed rhabdomyosarcoma, high-grade spindle cell sclerosing type, measuring 4.0 × 3.0 × 2.8 cm. Mitotic rate was 7/10 per HPF, and areas of fibrosis were consistent with chemotherapeutic response. Margins were negative for tumor, and the tumor was 1 mm from the deep margin. Lympho-vascular invasion was not identified.
The patient received a course of adjuvant radiotherapy and has now recovered to full function with a well-healed surgical site (Fig. 4).

DISCUSSION
Rare in adults, RMS comprises less than 0.03% of all adult malignancies [7]. In pediatric populations, RMS is exquisently sensitive to chemotherapy and radiation [8]. On the other hand, the standard of care in adult RMS is surgery and radiotherapy. Interestingly, our patient presented with a primary sc-RMS arising from a rectus myocutaneous flap used to close a previous traumatic defect, posing a challenge to achieve surgical cure while maintaining the patient’s lower extremity function and cosmesis. After resection of the tumor with negative margins, the defect was reconstructed with an ALT free flap, using the previous deep inferior epigastric pedicle as recipient vasculature, helping to preserve function in the patient’s lower extremity.
Molecular studies on our patient’s tumor demonstrated heterozygosity for the p.L122R mutation in MYOD1, which is known to be a somatic driver of sc-RMS [9]. MYOD1 is a transcription factor that regulates skeletal muscle differentiation, and mutations alter its function resulting in enhanced proliferation and impaired myogenic differentiation [9]. Unfortunately, patients carrying the p.L122R mutation in MYOD1 have an exceptionally poor prognosis, with 55% of cases demonstrating local recurrence and 55% of cases demonstrating distant recurrence after 28 months of follow-up [3]. Moreover, these tumors are less susceptible to chemotherapy than other histologic subtypes of RMS, making this disease especially lethal. It is crucial to characterize the molecular subtype of RMS, with MYOD1-mutant sc-RMS being a particularly aggressive disease. In the present case, our patient is in remission 9 months after surgical treatment with negative margins and ongoing chemotherapy.
Others have described successful recycling of the previous pedicle to act as the recipient for a new free flap [10]. Our case demonstrates proof of vascular integrity and continued patency of the original pedicle to re-perfuse the newly transferred ALT-free flap. To our knowledge, this is the first case in the literature describing a primary sarcoma arising within a previous free flap. In this case, we were able to adequately resect the tumor and reconstruct the area while maintaining perfusion to the distal lower extremity by utilizing the previous flap pedicle as a recipient for our free flap reconstruction.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



