-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammad Jarrah, Mohamad Mokadem, Pharmaco-endoscopic therapy for weight regain post-gastric bypass: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 2, February 2023, rjad075, https://doi.org/10.1093/jscr/rjad075
Close - Share Icon Share
Abstract
About 1 in every 4 patients who undergo bariatric surgery regains significant amount of weight some time along their journey, posing it as a serious problem that needs to be addressed in a pandemic of obesity. Lifestyle modification, anti-obesity medications, and bariatric endoscopy are multiple therapeutic options that can be used to support any weight loss attempt. A 53-year-old woman with morbid obesity who responded adequately to gastric-bypass regained significant weight 8 years later. We initially approached her post-operative weight regain in a behavioral, pharmacologic non-invasive manner; however, she failed to appropriately respond to several anti-obesity medications. Upper endoscopy revealed a dilated gastric pouch and gastro-jejunal anastomosis (GJA) that was reduced using argon plasma coagulation (APC), but also with a modest response. We then added liraglutide to her APC endo-therapy sessions and subsequentially patient started losing significantly more weight. For selective post-bariatric surgery weight re-gainers, endoscopic and pharmaco-therapy combined may be needed for more effective results.
INTRODUCTION
Obesity is well known to be a major contributor to the development of heart disease, stroke and cancer, which are the leading causes of death in the United States of America and around the world [1]. The prevalence of obesity among American adults rose from 33.7% in 2007 to 42.4% in 2018, and could reach around 50% by 2030, according to predictive models [2–4]. This disease carries a huge burden and is associated with multiple comorbidities, including type 2 diabetes, hypertension and non-alcoholic fatty liver disease [5]. This has urged all public health sectors to develop multiple preventive measures and comprehensive treatment approaches to address this global health problem [6].
Bariatric surgery is currently the most effective and durable therapy offered to patients with morbid obesity with laparoscopic sleeve gastrectomy (LSG) and Roux-en-Y gastric bypass (RYGB) being the two most performed bariatric procedures worldwide [7]. Despite the high rate of initial weight loss response, averaging ~66% excess weight loss (EWL) for RYGB and 56% EWL for LSG at 1 year, about 25% of patients who underwent either procedure regain most of their weight lost within 10 years post-surgery [8]. Regaining weight after bariatric surgery can be devastating as many of the obesity-related comorbidities can recur, and patients may become psychologically depressed as they may feel that they have failed the last resort available [9]. Fortunately, a variety of treatment modalities exist, ranging from psycho- and pharmacotherapy to endoscopic and surgical interventions, that can help weight re-gainers go back on track [8, 10]. Post-operative anatomical changes, such as gastro-jejunal anastomosis (GJA) dilation, have been associated with weight regain after RYGB. In addition, genetic, psychological, nutritional, and behavioral factors play a role, making weight regain a multifactorial process [11, 12]. Endoscopic therapy as well as several anti-obesity medications have already been used to manage post-bariatric surgery weight regain [13]. Here we present the case of a patient who had adequate weight loss following RYGB but subsequently regained a lot of it 8 years later. She had suboptimal response with conventional therapy with either medication or endoscopic therapy, alone.
CASE REPORT
A 53-year-old woman with class 3 obesity and hypertension underwent laparoscopic RYGB in 2007. Her pre-operative weight was 132.3 kg with a BMI of 47.1. She lost a maximum weight of 46.4 kg and weighed 85.9 kg at 1-year post-surgery. She mentioned that she gained a few kilograms and stabilised between 92 and 94 kg for ~8 years. In November 2015, she was evaluated for abdominal pain and weighed 101.2 kg. An Esophagogastroduodenoscopy (EGD) performed at that time showed normal RYGB anatomy, including a normal appearing GJA (Fig. 1). The patient reported occasional binge eating due to emotional stress. She declined psychotherapy and did not follow-up with dietary recommendations or lifestyle advice provided to her at that time. The patient continued to gain weight without seeking medical attention, reaching a peak post-operative weight of 115.4 kg in February 2017.
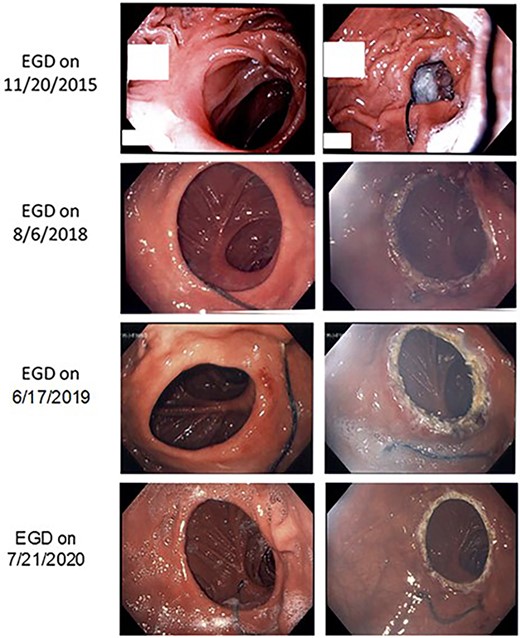
Images are shown during EGD at different time periods. The left panel shows pre-intervention, and the right panel shows post-APC intervention (no intervention on 20 November 2015).
She then decided to address her weight gain as it began to affect her quality of life. She enrolled in a weight management program where she was given advice and guidance on healthy food selection, calorie tracking, timing of meals, exercise and sleep. She was also started on phentermine/topiramate in February 2017. After 4 months, she had lost 1.1 kg, but reported minimal appetite suppression from the medication. Therefore, she was switched from phentermine/topiramate to lorcaserin, which was FDA-approved at the time, but only lost 1.4 kg in 3 months. We went over the patient’s diary regimen and found that the patient took the medication for less than 2 months effectively, so we increased the lorcaserin dose to the maximum. Nonetheless, she still had a modest weight loss response of 2.3 kg after 3 months.
Metformin was added to her treatment regimen in December 2017. After 3 months, she lost an additional 1.8 kg but due to gastrointestinal symptoms, she decided to discontinue both medications. We then started her on liraglutide 0.6 mg daily in July 2018 instead while planning for an EGD on her in August 2018. Surprisingly, she gained 4.3 kg during that month on liraglutide, so she decided to stop it. Her EGD showed a mildly dilated pouch (~ 7 cm) and a dilated GJA at ~40 mm in diameter, which was treated endoscopically by APC to promote GJA reduction (Fig. 1). After 4 months, the patient had lost 3.6 kg, which was still considered suboptimal. After further discussion with the patient, liraglutide was resumed at an escalated dose from 0.6 to 3 mg over a 16-weeks period. After 6 months, the patient weighed 6.6 kg less than her previous visit. She underwent a second endoscopic treatment in June 2019 when the GJA was still partially dilated at ~30 mm in diameter, and she was again treated by APC (Fig. 1). She had a 1-year follow-up and weighed 99.1 kg while still on liraglutide 3 mg daily. Her EGD in July 2020 showed a GJA of ~25 mm in diameter, which was treated with APC as before (Fig. 1). During her last follow-up visits in July 2021 and January 2022, the patient weighed 94.1 and 95 kg, respectively, and was still tolerating well liraglutide 3 mg daily (Fig. 2). She lost a maximum of 19 kg (16.8%) while on the combination of endoscopic and pharmacologic therapy and maintained it for ~1.5 years.
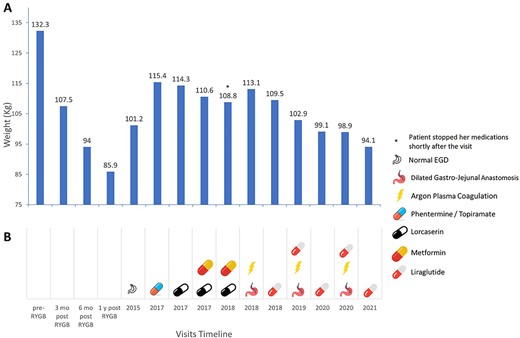
(A) Weight change during her visits after RYGB in 2007. (B) Different interventions at each timeline (pharmacologic/endoscopic).
DISCUSSION AND CONCLUSION
Retrospective studies demonstrate that pharmacotherapy, including phentermine/topiramate, lorcaserin, and naltrexone/bupropion, induce a total weight loss of 5–15% in patients with inadequate weight loss or weight regain after bariatric surgery [7, 14]. Moreover, a recent prospective study shows that patients with weight regain during more than 6 years after RYGB lose an average of 15% of total body weight in response to liraglutide treatment after 24 months, similar to surgery naif patients [15, 16].
APC is a non-contact electrocoagulation method that uses radiofrequency energy to induce superficial thermal coagulation on the applied tissue. This treatment aims to reduce the GJA dilation in post-RYGB patients gaining weight [17–19]. A recent retrospective study showed that APC is effective in the treatment of weight regain after RYGB and interestingly, and higher-watt APC was associated with greater weight loss [20].
Endoscopic full-thickness suturing is another useful modality for inducing endoscopic trans-oral outlet reduction to control weight regain after RYGB, and some studies have shown that performing APC prior to suturing leads to a greater weight loss [21]. However, recent studies have shown that APC alone is similar to APC in combination with full-thickness suture in terms of weight loss outcomes in patients with weight gain after RYGB [22, 23]. Most of these studies suggest that 6–10% of the overall body weight loss may result from endoscopic treatment at 12 months [19, 21].
Multiple drug regimens including phentermine/topiramate, lorcaserin, and metformin were used by our patient, but only minimal weight loss was achieved (4% overall body weight loss). However, the combination of APC and liraglutide resulted in an overall body weight loss of 16.8%, reaching a body weight like 6 months post-RYGB. This may be the first case reporting the efficacy of combining endoscopic revisional therapy with APC and pharmacotherapy for post-RYGB weight regain, after inadequate weight response to either treatment alone.
This suggests that the response to post-bariatric surgery weight regain management is variable and needs to be individualised by trial and error and patient’s preference until we have better understanding of personalised medical conditions.
ACKNOWLEDGEMENT
Authors would like to thank Dr. Yi Chu for his critical revision of the manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest related to the content of this manuscript.
FUNDING
This work was supported by grants from the US Veterans Merit Award (#I01 BX004774 and #I01 BX005173) MM. The contents do not represent the views of the U.S. Department of Veterans Affairs or the U.S. Government.
DATA AVAILABILITY
All data related to this manuscript are patient-protected and are available upon request by contacting the corresponding author.
REFERENCES
Kim TY, Kim S, Schafer AL. Medical management of the postoperative bariatric surgery patient. In: Feingold KR, Anawalt B, Blackman MR, et al., eds. Endotext. South Dartmouth (MA): MDText.com, Inc., 2000.
- obesity
- weight reduction
- upper gastrointestinal endoscopy
- endoscopy
- anastomosis, surgical
- anti-obesity agents
- argon
- blood coagulation
- gastric bypass
- obesity, morbid
- plasma
- surgical procedures, operative
- jejunum
- pharmacology
- bypass
- lifestyle changes
- coagulation process
- bariatric surgery
- gastric bypass, roux-en-y
- pandemics
- weight-loss agents
- liraglutide



