-
PDF
- Split View
-
Views
-
Cite
Cite
Paul William Itule Lugwaja, Yona Ringo, Godfrey Mchele, Gabriel Mtaturu, An extremely rare neoplasm ‘atypical spindle cell pleomorphic lipomatous tumor’: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 2, February 2023, rjad040, https://doi.org/10.1093/jscr/rjad040
Close - Share Icon Share
Abstract
Spindle cell lipoma is a rare histological variant of lipoma accounting for 1.5% of adipocytes tumors. It is composed of an admixture of mature adipocytes and fibroblast-like spindle cells in a myxoid stroma. Retroperitoneal atypical spindle cell lipomatous tumor are extremely rare only a single report in the literature reported. Herein we describe a case of a giant lipomatous tumor that was causing partial bowel obstruction. Successful excision with en block resection of the tumor, distal ureter and posterior wall of the bladder was achieved by teamwork between gastrointestinal surgeons and Urologist. The bladder defect was repaired, and left ureteric reimplantation was done. The patient made a good recovery with excellent progress. He has resumed his normal activities as a farmer.
INTRODUCTION
Lipomas are the most frequent soft tissue tumors in adults worldwide. They are termed as a collection of proliferating matured fat cells, encapsulated by a thin fibrous tissue. Lipomas are generally benign tumors [1]. Spindle cell lipoma differs from liposarcoma because it does not contain lipoblasts and lacks MDM2 and CDK4 amplification [2, 3].
ASPLT typically arises from soft subcutaneous tissues of extremities, shoulder, head, neck region and in the deep soft tissue of extremities. It is unusual in gastrointestinal organs and very unusual in the retroperitoneum tissues [2, 4]. Intra-abdominal ASPLT is mostly seaming to affect mainly men between 45 and 60 years of age [5].
ASPLT is a modern category of adipocytic tumors that were not in history till 1994 when Dei Tos and others described six ASPLT neoplasms they were initial named spindle cell liposarcoma [6] and then later regarded as a variant of well-differentiated liposarcoma, which is potentially low-grade malignant mesenchymal neoplasms with a high propensity to local recurrence and tendency to differentiate to higher grades over time [7, 8].
CASE REPORT
Presentation
A 52-year-old male was admitted to our hospital with a history of progressive abdominal distension for 10 months associated with early satiety, abdominal pain, constipation, bilateral lower limb edema, orthopnea and unintentional weight loss. He had no constitutional symptoms, history of cigarette smoking, history of alcohol intake, radiation exposure, or abdominal trauma and no similar condition in the family.
Physical examination findings were as follows: BP 136/86 mmhg, PR 78 bpm, SPO2 98%, RR 16 cpm, temperature 36.9°C, with lower limb edema.
The abdomen was symmetrically distended and moved with respiration. He had mild tenderness throughout the abdomen. A huge mass was palpated from the xiphoid to the symphysis pubis, occupying the central region of the abdomen. It was firm and immobile, and other systemic examinations were unremarkable (Fig. 1).

Gross appearance showing generalised abdominal distention with marked wasting.
INVESTIGATION
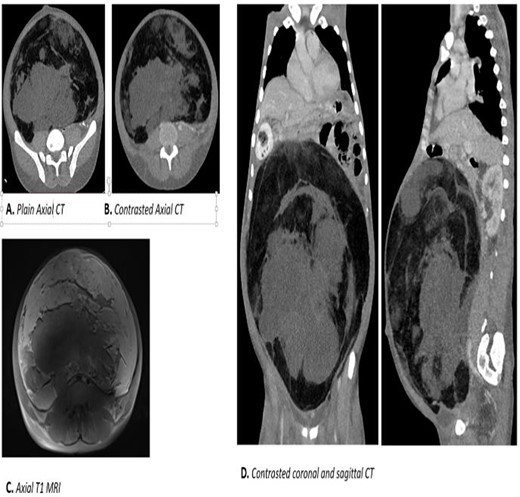
Laboratory results were normal except for microcytic hypochromic anemia with hypoalbuminemia of 2.4 mg/L (Fig. 2):
Abdominal and pelvic MRI: showed a huge mass from the pelvis extending to the abdomen measuring approximately 17 × 26 cm2.
Abdominal-pelvic CT-Scan: a large solid mass measuring 35.91 × 31.83 cm2 displacing the viscera and causing bilateral hydronephrosis.
TREATMENT
The patient was optimised for surgical excision and elective laparotomy was done thereafter. Intraoperatively, we noted a huge retroperitoneal tumor from the pelvis to the xiphoid. Other intra-abdominal organs were normal. Bowels were displaced, and the bladder was pushed cranially and to the right.
The tumor did not invade the adjacent organs except the intimate adherence to the distal part of the bladder posterior and superior laterally. A mixture of blunt and sharp dissection plus cauterisation was used to mobilise and release the tumor.
During the tough dissection, the distal left ureter and portion of the posterior wall of the urinary bladder were unavoidably injured. The left ureter was directly replanted to the urinary bladder with a double J (pigtail) ureteric stent and the urinary bladder was repaired in two-layer technique. En block excision of the tumor was done and histology confirmed negative margins.
Postoperatively, the patient was admitted to ICU where he stayed for 2 days. We retained the Foley urethral catheter for 14 days as a standard procedure following bladder repair. The patient developed a urine leak that was captured by abdominal drain. It was managed conservatively and completely resolved by day 12. He was discharged on day 16 after surgery. The ureteric stent was removed after 6 weeks (Fig. 3).
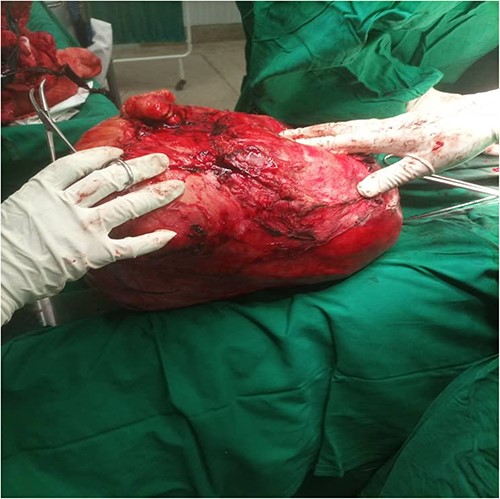
Intraoperative en bloc excision of a large intraabdominal mass originating from the posterior wall of the urinary bladder.
Pathology results
A substantial capsulated mass, measuring 35 × 25 × 12 cm3, no other structure accompanied the mass.
Microscopic: on the assessment of a well-differentiated tumor, displaying mature adipocytes, with some spindle cells, that were bland and many hyalinised collagen fibers. There were also scatted multinucleated giant cells. Floret cells were noted with some lipoblast. Myxoid stroma.
Immunohistochemistry: CD 34 positive and Ki67 negative.
Conclusion: atypical spindle cell pleomorphic lipomatous tumors (Fig. 4).

(A) Low power: paracellular tissue with collagenous stroma. (C) Intermediate power: fibrofatty tissue with abundant hyaline-like fibro collagenous fibers and mature adipocytes, scant scattered hyperchromatic cells. Arrow showing a visible giant floret cell. (B, D) High power: mature adipocytes of variable size, scattered hyperchromatic spindle cells and mast cells as well as large prominent giant floret cells (Dr Atuganile Malango, Dr Fadia Ali).
DISCUSSION
In 2020, the World Health Organization reviewed the nomenclature of spindle cell liposarcoma and assigned a new term ‘Atypical Spindle cell Pleomorphic Lipomatous Tumor’. It was recognised as a new entity for the group of benign, low-grade adipocytic neoplasms [9]. The tumor pathologically has features atypical spindle cells, multi-nucleated cells, pleomorphic lipoblasts and poor circumscription [6].
Most of the ASPLT occurs in a middle-aged person with a male preponderance. It is commonly diagnosed on the distal extremities; however, few cases had been reported on the neck, head, tongue and genitalia. The ASPLT is commonly originating from the subcutaneous [10]. Intra peritoneal ASPLT is rare in literature and reported in the appendix and intra-abdominal esophagus [10–13].
Retroperitoneal ASPLT is extremely rare only a single report in the literature reported from an 18-year-old male patient [14]. To the best of our knowledge, we are reporting the second case of pathologically confirmed retroperitoneal ASCPLT in literature diagnosed from a 52-year old male. He had no cough, blood in the stool or excessive night sweating. This presentation is similar to what was found in the first previous case report by Jung-Min et al [14].
Definitive treatment of the ASPLT tumor is complete R0 resection confirmed this was achieved in our case by en block resection of the mass with a segmental of the distal left ureter and lateral poster wall of the urinary bladder. We are expecting an excellent prognosis in our patient with recurrent rates of less than 10–15% [6, 12].
In most ASPLT cases, the degree of nuclear atypia in the spindle cell component is focal and varies from mild to moderate. In addition to that, dispersed multinucleated and pleomorphic cells are identified within the adipocytic or spindle cell components. Rarely, mitosis is expressed, and there is an absence of tumor necrosis [13].
In our case, we found mature adipocytes, some spindle cells and many hyalinised collagen fibers. Numerous scatted multinucleated giant cells, and few lipoblasts are present. Most ASPLT cases are linked to the deletion or loss of RB1 and absent MDM2 or CDK4 amplification.
REFERENCES
Lecoutere E, Creytens D.



