-
PDF
- Split View
-
Views
-
Cite
Cite
Kai Tang, Yong-bao Zhang, Jie Fang, Tao Shi, Chen-yang Shen, Iatrogenic arteriovenous fistula after lumbar discectomy surgery: a case report, Journal of Surgical Case Reports, Volume 2023, Issue 2, February 2023, rjac576, https://doi.org/10.1093/jscr/rjac576
Close - Share Icon Share
Abstract
Iatrogenic arteriovenous fistula (IAVF) is an unusual and potentially fatal complication of lumbar spinal surgery. A 62-year-old patient presented with a history of dyspnea, left lower limb edema and coughing. A physical exam showed bilateral basal rales in the lungs, abdominal bruit and bilateral lower limb pitting edema. A computed tomography angiograph revealed an arteriovenous communication between the right internal iliac artery and the left common iliac vein. The patient was diagnosed with an IAVF, which developed post-lumbar disc surgery. The patient underwent a successful endovascular treatment by using covered stent at the common iliac artery with embolism of lumbar artery. The patient’s symptoms were relieved 2 months after surgery.
INTRODUCTION
Iatrogenic vascular injury is a rare complication of lumbar spine surgery. The incidence of vascular complications is ~0.04% [1]. According to reports, the mortality rate is ~15–61% [2]. Complications of vascular injury mainly include vascular lacerations, arteriovenous fistulas and pseudoaneurysms. Arteriovenous fistula between the right internal iliac artery and the left common iliac vein is extremely rare compared with other complications. Arteriovenous fistulas has atypical clinical symptoms, which is easy to be misdiagnosed [3].
We report one case of iatrogenic AVF between the right internal iliac artery and the left common iliac vein, which occurred secondary to lumbar spinal surgery and was treated with an endovascular stent graft.
CASE REPORT
A 62-year-old man was admitted to our hospital with a history of dyspnea, left lower limb edema and coughing for 15 years. The past clinical history was a discectomy surgery at L4–L5 level 15 years ago. There was no relevant family history.
He had multiple hospital admissions with left lower limb edema and heart failure. He was diagnosed with deep vein thrombosis and pulmonary hypertension in the local hospital. On admission, clinical examination revealed bilateral basal rales in the lungs and abdominal bruit. The blood biochemical indexes were NT-proBNP 1075 pg/ml, and other biochemical indexes were within the normal range. Echocardiography demonstrated showed a severely dilated right ventricle. Chest X-ray revealed lung infection and pulmonary hypertension. Computed tomography angiography (CTA) showed there was an AVF between the right internal iliac artery and the left common iliac vein and dilated tortuous veins in the left lower limb (Fig. 1).

CTA showing AVF between the right internal iliac artery and the left common iliac vein. (A) The left common iliac vein and dilated tortuous veins in the left lower limb; (B, C) An AVF (black arrow) between the right internal iliac artery and the left common iliac vein.
After multi-disciplinary team consideration, we decided to enclose the AVF by using covered stent at the right common iliac artery. Through a percutaneous right femoral approach, one covered stent graft (16–10–100 mm Medtronic) was implanted at the right common iliac artery. Angiography demonstrated that the contrast can pass into the inferior vena cava. We decided to embolized the lumbar artery by coils through the femoral approach to prevent the contrast passing into the venous system (Fig. 2). Completion angiography demonstrated a significant improvement. Symptoms alleviated quickly after successful endovascular treatment. One month later, left lower limb edema disappeared completely. After 12 months of follow-up, there were no complications occurred in the patient.
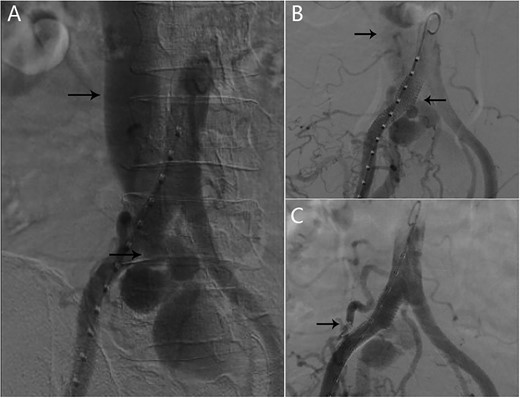
(A) AVF and inferior vena cava can be seen in the angiography; (B) one covered stent graft was implanted at the right common iliac artery; angiography demonstrated that the contrast can pass into the inferior vena cava; (C) after the lumbar artery was embolized by coils, inferior vena cava was no longer enhanced.
DISCUSSION
AVFs are an abnormal communication between an artery and a vein. AVFs secondary to lumbar spinal surgery were rarely reported. The aorta and the inferior vena cava usually run on the right side of the spine. The aorta is divided into bilateral common iliac arteries at the level of the fourth lumbar vertebra [4]. The common iliac vein merges into the inferior vena cava at the level of the fourth lumbar vertebra. The common iliac artery is generally located in front of the fourth and fifth lumbar vertebrae. When the anterior longitudinal ligament is penetrated during lumbar spine surgery, it is easy to cause blood vessel damage. The most common vascular injury in L4–S1 lumbar spine surgery is the iliac artery and vein. In higher lumbar spine surgery, such as L1–L2 and L2–L3, abdominal aorta injuries are more common [5].
AVF presents with symptoms of cardiac failure including edema, dyspnea and abdominal distention. Nonspecific symptoms in iliac AVF cause delayed diagnosis. Most patients with arteriovenous fistulas were diagnosed >1 month after surgery. When an arteriovenous fistula is formed, there will be an abnormal channel shunts left to right. The blood in the arteries flows from the high-pressure side to the low-pressure side, causing the right heart volume overload [2]. Long-term left-to-right shunt leads to the development of secondary pulmonary hypertension and right heart failure. It is extremely important for the early diagnosis of iatrogenic arteriovenous fistula (IAVF). Therefore, if the patient has abdominal discomfort after lumbar spine surgery, IAVF should be considered.
Angiography is the gold standard in the diagnosis of AVF. However, enhanced computed tomography (CT) can be used as alternative noninvasive imaging techniques to diagnose vascular fistula. Enhanced CT can be helpful in the diagnosis as well as in planning the treatment of AVF.
Surgical treatment in iliac AVF carries high mortality and morbidity rates. Endovascular treatment has the advantages about less trauma, short anesthesia time, quick post-operative recovery and short hospital stay [6]. In our case, long-term left-to-right shunt led to the development of secondary pulmonary hypertension and right heart failure. Endovascular treatment was a safe and appropriate method for our patient.
In conclusion, doctors should be alert to IAVF during lumbar disc surgery. In patients presenting with atypical clinical symptoms in the context of surgery, it is important to consider IAVF as a rare differential diagnosis. Following the rapid development of endovascular techniques, majority of these iatrogenic vascular injury can choose minimally invasive therapeutic options.
CONFLICT OF INTEREST STATEMENT
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
FUNDING
None.
DATA AVAILABILITY
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.



