-
PDF
- Split View
-
Views
-
Cite
Cite
Osamu Shimooki, Naoko Ito, Masanori Hakozaki, Yukihiro Minakawa, Chihiro Tono, Tadashi Abe, A sewing needle in the liver: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad678, https://doi.org/10.1093/jscr/rjad678
Close - Share Icon Share
Abstract
Intrahepatic foreign bodies are rarely reported. Although rare, a few reports of swallowed foreign bodies straying into the liver from the gastrointestinal tract have been published. Herein, we report a case in which an asymptomatic intrahepatic needle was removed laparoscopically. An 81-year-old woman presented to our hospital with an abnormal shadow on her abdominal X-ray image. Abdominal computed tomography displayed a needle-like shadow obliquely lying in the lateral segment of the left lobe of the liver. No subjective symptoms were reported; however, the patient underwent laparoscopic extraction. The postoperative course was good, and the patient was discharged without any complications. We also present a literature review of 27 patients with intrahepatic foreign bodies, a sewing needle.
Introduction
In addition to the percutaneous route of intrahepatic foreign body entry, cases of accidentally swallowed foreign bodies migrating to the liver through the gastrointestinal tract have been reported. In general, several foreign bodies, even sharp ones, are spontaneously excreted; however, a few require surgical treatment because of gastrointestinal tract perforation. Although extremely rare, a few foreign bodies have been reported to remain in the parenchymal organs, such as the liver and pancreas [1, 2]. Herein, we describe a case in which a sewing needle that appeared to have migrated from the gastropyloric region into the liver was safely removed via laparoscopic surgery.
Case report
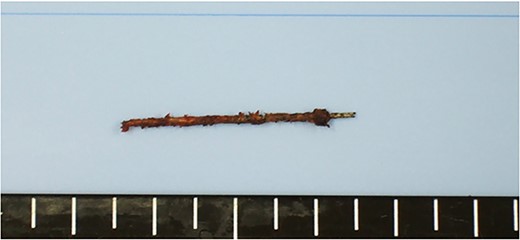
An 81-year-old woman presented to our hospital with an abnormal shadow on her abdominal X-ray performed during a gastrointestinal checkup. She had no subjective symptoms. She had no comorbidities other than hypertension and no history of laparotomy. Her vital signs were normal. No foreign body was palpable on the abdominal wall, chest wall, or back. No mental abnormality or cognitive impairment was noted. A plain abdominal radiograph showed a needle-like shadow at the second lumbar vertebra level (Fig. 1). Abdominal computed tomography (CT) displayed a needle-like shadow obliquely directed from the inferior surface of the liver to the lateral segment. No intrahepatic or intraperitoneal abscess was observed (Fig. 2). Upper gastrointestinal endoscopy revealed no stomach or duodenal ulcer scarring. Detailed history revealed no history of trauma or acupuncture treatment and no memory of accidental ingestion of needles. No subjective symptoms such as sore throat or epigastric pain were reported. Based on these findings, a sewing needle was accidentally swallowed without awareness, perforating at the pylorus of the stomach or duodenal bulb and straying into the liver. The patient had no symptoms at the time of the visit, and we told her that she could be followed up. However, the patient strongly desired needle removal; therefore, we decided to perform a laparoscopic resection. Laparoscopic observation revealed fibrous adhesion between the lesser curvature of the gastric pylorus and the inferior surface of the outer hepatic segment. When the adhesion was detached, the foreign body tip was observed on the subhepatic surface. It was grasped with forceps, extracted, and removed from the abdominal cavity (Fig. 3). A sewing needle of ~3-cm length was removed (Fig. 4). The patient had a good postoperative course and was discharged from the hospital on postoperative Day 4 without any complications.

Plain abdominal radiograph displaying a needle-like metallic shadow at the second lumbar vertebral level.
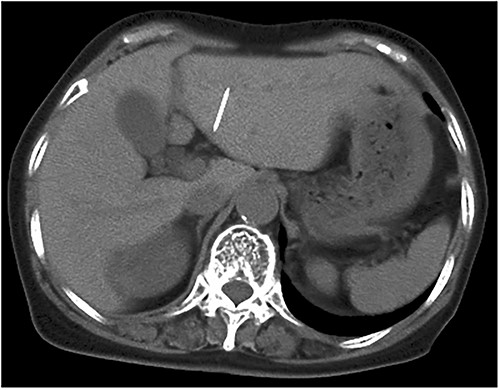
Abdominal CT scan displaying needle-like shadows obliquely lying in the left lateral segment of the liver.

Extraction of the foreign body from the liver under laparoscopy surgery
Discussion
Percutaneous or transgastrointestinal routes are common routes of entry for intrahepatic foreign bodies, although percutaneous entry can be easily identified from the patient’s history. A history of accidental ingestion via the transgastrointestinal route may be clear or unclear. In general, most mislabeled foreign bodies are transanally expelled. However, a few bodies require surgical treatment because of gastrointestinal tract perforation, and although rare, foreign bodies are found after migrating from the gastrointestinal tract to neighboring organs [1, 3]. Sharp and long intrahepatic foreign bodies, such as fish bones, toothpicks, chicken bones, pens, and sewing needles, have been reported [4]. Among these, sewing needles are very rare, with only 27 cases reported, including this case (Table1). Of the reported cases, 15 (56%) were females and 8 (30%) were children <14 years. In total, 3 cases (11%) were obviously ingested, and 12 cases (44%) were asymptomatic and discovered by chance. Of the 12 cases (44%) with symptoms such as abdominal pain, 5 (19%) had liver abscesses. Fish bones are often detected as liver abscesses [5], whereas sewing needles are characterized by the fact that several patients are asymptomatic. In the case of sewing needles, asymptomatic patients can be followed up with the appearance of symptoms, such as abdominal pain and fever, and with imaging studies. In fact, five cases (19%) were followed up without intervention, and long-term asymptomatic cases without position changes have been reported [6, 7]. The foreign body was most frequently located in the right lobe of the liver in 14 cases (52%), the left lobe in 11 cases (41%), and the caudate lobe in 2 cases (7%). Surgery was performed in 22 patients (81%). Although laparotomy was necessary in a few cases because of acute abdomen or liver abscess [8, 9], laparoscopic surgery, which is less invasive, was performed in nine cases (33%). In this case, the patient was asymptomatic and could have been conservatively followed-up; however, because the patient wished to undergo surgery, a laparoscopic excision was performed. The postoperative course was excellent, and the patient was able to leave the hospital postoperative Day 4. The choice of surgical technique depends on the patient’s coexisting medical conditions, and laparoscopic resection was considered an appropriate technique. When laparoscopic surgery is used, a preoperative CT scan is recommended to predict the location of the foreign body, and intraoperative ultrasound may be useful if the foreign body is located deep in the liver parenchyma [10, 11].
| Author . | Age . | Sex . | Diagnosis of needle . | Location . | Intervention . |
|---|---|---|---|---|---|
| Abel, 1971 | 11 years | Male | Incidental | Left lobe | Laparotomy |
| Urakami, 1993 | 51 years | Male | Abdominal pain | Left lobe | Laparotomy |
| Crankson, 1997 | 2 years | Male | Incidental | Right lobe | Observation |
| Saviano, 2000 | 65 years | Female | Abdominal pain | Left lobe | Videolaparoscopic removal |
| Roca, 2003 | 85 years | Female | Incidental | Right lobe | Observation |
| Chintamani, 2003 | 26 years | Male | Liver abscess | Right lobe | Laparotomy |
| Rahalkar, 2003 | 23 years | Female | Incidental | Right lobe | Observation |
| Nishimoto, 2003 | 1 years | Male | Incidental | Left lobe | Laparotomy |
| Aigrain, 2004 | 11 months | Male | Swallowing history | Right lobe | Laparoscopic removal |
| Lanitis, 2007 | 35 years | Female | Swallowing history | Left lobe | Laparoscopic and endoscopic |
| Azili, 2007 | 14 years | Female | Liver abscess | Right lobe | Laparotomy |
| Feng, 2009 | 76 years | Female | Incidental | Left lobe | Observation |
| Varetto, 2009 | 39 years | Male | Abdominal pain | Left lobe | Laparoscopic removal |
| Avcu, 2009 | 16 years | Female | Liver abscess | Right lobe | Laparotomy |
| Dominguez, 2009 | 3 years | Male | Incidental | Caudate lobe | Laparotomy |
| Jutte, 2010 | 45 years | Female | Liver abscess | Right lobe | Laparoscopic removal |
| Senol, 2010 | 27 years | Male | Incidental | Right lobe | Observation |
| Bolanaki, 2010 | 21 years | Male | Incidental | Caudate lobe | Laparotomy |
| Bulakçı, 2011 | 22 years | Female | Swallowing history | Right lobe | Laparoscopic removal |
| Incedayi, 2012 | 52 years | Female | Abdominal pain | Left lobe | Laparotomy |
| Bakal, 2012 | 14 years | Male | Abdominal pain | Right lobe | Laparotomy |
| Xu, 2013 | 5 months | Male | Incidental | Right lobe | Laparotomy |
| Deveci, 2014 | 15 years | Female | Abdominal pain | Right lobe | Laparotomy |
| Bostanci, 2017 | 22 years | Female | Incidental | Right lobe | Laparoscopic removal |
| Carver, 2018 | 32 years | Female | Dysphagia | Left lobe | Laparoscopic removal |
| Basquez, 2020 | 74 years | Female | Liver abscess | Left lobe | Laparotomy |
| Shimooki, 2023 | 81 years | Female | Incidental | Left lobe | Laparoscopic removal |
| Author . | Age . | Sex . | Diagnosis of needle . | Location . | Intervention . |
|---|---|---|---|---|---|
| Abel, 1971 | 11 years | Male | Incidental | Left lobe | Laparotomy |
| Urakami, 1993 | 51 years | Male | Abdominal pain | Left lobe | Laparotomy |
| Crankson, 1997 | 2 years | Male | Incidental | Right lobe | Observation |
| Saviano, 2000 | 65 years | Female | Abdominal pain | Left lobe | Videolaparoscopic removal |
| Roca, 2003 | 85 years | Female | Incidental | Right lobe | Observation |
| Chintamani, 2003 | 26 years | Male | Liver abscess | Right lobe | Laparotomy |
| Rahalkar, 2003 | 23 years | Female | Incidental | Right lobe | Observation |
| Nishimoto, 2003 | 1 years | Male | Incidental | Left lobe | Laparotomy |
| Aigrain, 2004 | 11 months | Male | Swallowing history | Right lobe | Laparoscopic removal |
| Lanitis, 2007 | 35 years | Female | Swallowing history | Left lobe | Laparoscopic and endoscopic |
| Azili, 2007 | 14 years | Female | Liver abscess | Right lobe | Laparotomy |
| Feng, 2009 | 76 years | Female | Incidental | Left lobe | Observation |
| Varetto, 2009 | 39 years | Male | Abdominal pain | Left lobe | Laparoscopic removal |
| Avcu, 2009 | 16 years | Female | Liver abscess | Right lobe | Laparotomy |
| Dominguez, 2009 | 3 years | Male | Incidental | Caudate lobe | Laparotomy |
| Jutte, 2010 | 45 years | Female | Liver abscess | Right lobe | Laparoscopic removal |
| Senol, 2010 | 27 years | Male | Incidental | Right lobe | Observation |
| Bolanaki, 2010 | 21 years | Male | Incidental | Caudate lobe | Laparotomy |
| Bulakçı, 2011 | 22 years | Female | Swallowing history | Right lobe | Laparoscopic removal |
| Incedayi, 2012 | 52 years | Female | Abdominal pain | Left lobe | Laparotomy |
| Bakal, 2012 | 14 years | Male | Abdominal pain | Right lobe | Laparotomy |
| Xu, 2013 | 5 months | Male | Incidental | Right lobe | Laparotomy |
| Deveci, 2014 | 15 years | Female | Abdominal pain | Right lobe | Laparotomy |
| Bostanci, 2017 | 22 years | Female | Incidental | Right lobe | Laparoscopic removal |
| Carver, 2018 | 32 years | Female | Dysphagia | Left lobe | Laparoscopic removal |
| Basquez, 2020 | 74 years | Female | Liver abscess | Left lobe | Laparotomy |
| Shimooki, 2023 | 81 years | Female | Incidental | Left lobe | Laparoscopic removal |
| Author . | Age . | Sex . | Diagnosis of needle . | Location . | Intervention . |
|---|---|---|---|---|---|
| Abel, 1971 | 11 years | Male | Incidental | Left lobe | Laparotomy |
| Urakami, 1993 | 51 years | Male | Abdominal pain | Left lobe | Laparotomy |
| Crankson, 1997 | 2 years | Male | Incidental | Right lobe | Observation |
| Saviano, 2000 | 65 years | Female | Abdominal pain | Left lobe | Videolaparoscopic removal |
| Roca, 2003 | 85 years | Female | Incidental | Right lobe | Observation |
| Chintamani, 2003 | 26 years | Male | Liver abscess | Right lobe | Laparotomy |
| Rahalkar, 2003 | 23 years | Female | Incidental | Right lobe | Observation |
| Nishimoto, 2003 | 1 years | Male | Incidental | Left lobe | Laparotomy |
| Aigrain, 2004 | 11 months | Male | Swallowing history | Right lobe | Laparoscopic removal |
| Lanitis, 2007 | 35 years | Female | Swallowing history | Left lobe | Laparoscopic and endoscopic |
| Azili, 2007 | 14 years | Female | Liver abscess | Right lobe | Laparotomy |
| Feng, 2009 | 76 years | Female | Incidental | Left lobe | Observation |
| Varetto, 2009 | 39 years | Male | Abdominal pain | Left lobe | Laparoscopic removal |
| Avcu, 2009 | 16 years | Female | Liver abscess | Right lobe | Laparotomy |
| Dominguez, 2009 | 3 years | Male | Incidental | Caudate lobe | Laparotomy |
| Jutte, 2010 | 45 years | Female | Liver abscess | Right lobe | Laparoscopic removal |
| Senol, 2010 | 27 years | Male | Incidental | Right lobe | Observation |
| Bolanaki, 2010 | 21 years | Male | Incidental | Caudate lobe | Laparotomy |
| Bulakçı, 2011 | 22 years | Female | Swallowing history | Right lobe | Laparoscopic removal |
| Incedayi, 2012 | 52 years | Female | Abdominal pain | Left lobe | Laparotomy |
| Bakal, 2012 | 14 years | Male | Abdominal pain | Right lobe | Laparotomy |
| Xu, 2013 | 5 months | Male | Incidental | Right lobe | Laparotomy |
| Deveci, 2014 | 15 years | Female | Abdominal pain | Right lobe | Laparotomy |
| Bostanci, 2017 | 22 years | Female | Incidental | Right lobe | Laparoscopic removal |
| Carver, 2018 | 32 years | Female | Dysphagia | Left lobe | Laparoscopic removal |
| Basquez, 2020 | 74 years | Female | Liver abscess | Left lobe | Laparotomy |
| Shimooki, 2023 | 81 years | Female | Incidental | Left lobe | Laparoscopic removal |
| Author . | Age . | Sex . | Diagnosis of needle . | Location . | Intervention . |
|---|---|---|---|---|---|
| Abel, 1971 | 11 years | Male | Incidental | Left lobe | Laparotomy |
| Urakami, 1993 | 51 years | Male | Abdominal pain | Left lobe | Laparotomy |
| Crankson, 1997 | 2 years | Male | Incidental | Right lobe | Observation |
| Saviano, 2000 | 65 years | Female | Abdominal pain | Left lobe | Videolaparoscopic removal |
| Roca, 2003 | 85 years | Female | Incidental | Right lobe | Observation |
| Chintamani, 2003 | 26 years | Male | Liver abscess | Right lobe | Laparotomy |
| Rahalkar, 2003 | 23 years | Female | Incidental | Right lobe | Observation |
| Nishimoto, 2003 | 1 years | Male | Incidental | Left lobe | Laparotomy |
| Aigrain, 2004 | 11 months | Male | Swallowing history | Right lobe | Laparoscopic removal |
| Lanitis, 2007 | 35 years | Female | Swallowing history | Left lobe | Laparoscopic and endoscopic |
| Azili, 2007 | 14 years | Female | Liver abscess | Right lobe | Laparotomy |
| Feng, 2009 | 76 years | Female | Incidental | Left lobe | Observation |
| Varetto, 2009 | 39 years | Male | Abdominal pain | Left lobe | Laparoscopic removal |
| Avcu, 2009 | 16 years | Female | Liver abscess | Right lobe | Laparotomy |
| Dominguez, 2009 | 3 years | Male | Incidental | Caudate lobe | Laparotomy |
| Jutte, 2010 | 45 years | Female | Liver abscess | Right lobe | Laparoscopic removal |
| Senol, 2010 | 27 years | Male | Incidental | Right lobe | Observation |
| Bolanaki, 2010 | 21 years | Male | Incidental | Caudate lobe | Laparotomy |
| Bulakçı, 2011 | 22 years | Female | Swallowing history | Right lobe | Laparoscopic removal |
| Incedayi, 2012 | 52 years | Female | Abdominal pain | Left lobe | Laparotomy |
| Bakal, 2012 | 14 years | Male | Abdominal pain | Right lobe | Laparotomy |
| Xu, 2013 | 5 months | Male | Incidental | Right lobe | Laparotomy |
| Deveci, 2014 | 15 years | Female | Abdominal pain | Right lobe | Laparotomy |
| Bostanci, 2017 | 22 years | Female | Incidental | Right lobe | Laparoscopic removal |
| Carver, 2018 | 32 years | Female | Dysphagia | Left lobe | Laparoscopic removal |
| Basquez, 2020 | 74 years | Female | Liver abscess | Left lobe | Laparotomy |
| Shimooki, 2023 | 81 years | Female | Incidental | Left lobe | Laparoscopic removal |
Conflict of interest statement
None declared.
Funding
None declared.



