-
PDF
- Split View
-
Views
-
Cite
Cite
Phelopatir Anthony, Tracey Edwards, Nagy Andrawis, Chronic sigmoid diverticulitis causing tubo-ovarian abscess and colo-uterine fistula, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad659, https://doi.org/10.1093/jscr/rjad659
Close - Share Icon Share
Abstract
Colo-uterine fistulas are rarely reported in the literature, and its presentation in the presence of a tubo-ovarian abscess secondary to chronic sigmoid diverticulitis is currently not reported. As such, its presentation may pose a diagnostic dilemma. Here, we present a 68-year-old woman who was admitted under the colorectal service with a 1 month history of mild left iliac fossa pain, with computed tomography (CT) demonstrating complicated sigmoid diverticulitis. Progress CTs, however, demonstrated a progressively enlarging left iliac fossa mass, with air fluid levels, densely adherent to the sigmoid colon. The decision was eventually made to perform a laparoscopy, which demonstrated a left tubo-ovarian abscess communicating with the uterus and sigmoid colon, illustrating a colo-uterine fistula. Open resection of the sigmoid colon and uterus was performed and the patient recovered uneventfully. This case describes an uncommon complication of chronic sigmoid diverticulitis and the importance of its judicious surgical management.
Introduction
Colo-uterine fistulas are a rare complication of sigmoid diverticulitis [1]. Although sigmoid diverticulosis is common in the western world, affecting 50% of individuals over the age of 50 [2], the most common complications of this pathology include perforation and pericolic abscess formation [3]. Fistula can also ensue from complicated diverticulitis, however, this mostly manifests as colo-vesical and colo-vaginal [4]. The rarity of colo-uterine fistulae is contributed to by the uterus’ thick myometrium [5]. Here, we describe a 68-year-old woman’s with colo-uterine fistula with tubo-ovarian abscess secondary to chronic sigmoid diverticulitis.
Case report
A 68-year-old woman presented to hospital with 1 month history of Left iliac fossa (LIF) pain and weight loss of 5 kg. She denied per vaginal (PV) discharge and urinary symptoms, and had no medical background nor a history of previous colonoscopies. On examination, she was haemodynamically stable, not in respiratory distress and was afebrile at 36.8°C. The patient demonstrated LIF tenderness but was not peritonitc. Laboratory results were significant for increased C-reactive Protein (CRP) of 185 mg/L, with normal white cell count (WCC) and normal tumour markers. Contrast enhanced computed tomography (CT) Abdomen/Pelvis, illustrated in Fig. 1, demonstrated a LIF mass measuring 3.9 cm × 3.4 cm × 2.9 cm in the area of the left ovary, abutting the sigmoid colon, containing both solid and cystic components, with appearances inconclusive for ovarian neoplasia or pericolic abscess. There was evidence of sigmoid diverticulosis without diverticulitis.
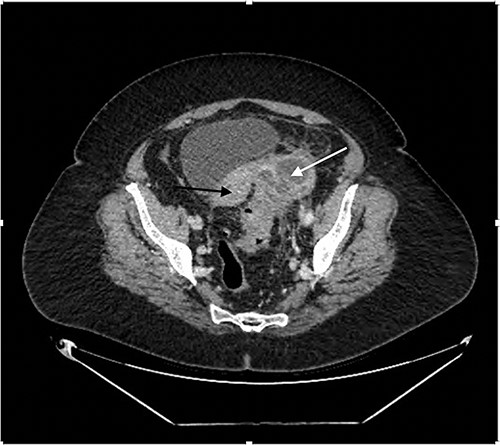
Contrast enhanced CT Abdomen/Pelvis demonstrating mixed cystic/solid LIF mass (white arrow) adherent to the sigmoid colon and uterus (black arrow).
The patient was admitted under the surgical team and commenced on intravenous antibiotics for 2 days, and then was discharged. Colonoscopy was then performed 2 weeks following discharge, revealing sigmoid diverticulosis, no polyps and no evidence of complicated diverticulitis, as demonstrated in Fig. 2.

Colonoscopy following first hospital admission, demonstrating evidence of sigmoid diverticular disease, with no evidence of fistula formation.
In 4 months, following an exacerbation of LIF pain, outpatient CT demonstrated the LIF mass had now progressed in size, up to 9.0 × 7.0 × 5.3 cm in dimension, with now multiple air fluid levels, accompanied with complete loss of the tissue planes between the lesion and the sigmoid colon. There was also free fluid in the Pouch of Douglas (POD), as seen in Fig. 3. As such, the conclusion was made that the patient had likely chronic Hinchey Class 2 diverticular abscess, requiring operative intervention.
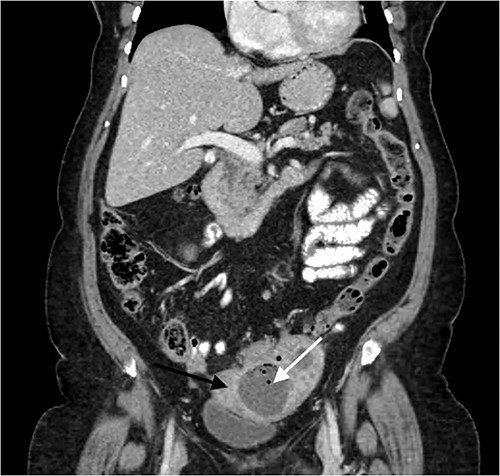
Contrast enhanced coronal CT Abdomen/Pelvis revealing a larger multi-loculated rim enhancing LIF mass (white arrow) adherent to the uterus (black arrow), with air fluid levels and multiple locules of gas.
The patient proceeded with a laparoscopy + anterior resection + proceed. Intra-operatively, the procedure was converted to open and a left tubo-ovarian abscess (TOA) was found to be communicating with the sigmoid colon and uterus, confirming colo-uterine fistula. A low anterior resection in addition to a subtotal hysterectomy was performed, whereby the uterus was resected en-bloc with the TOA. A defunctioning loop ileostomy was also performed. The patient underwent an uneventful recovery and was discharged home after 10 days. Her loop ileostomy was reversed 6 weeks later. Histopathology revealed a multi-loculated TOA, 80 × 70 × 45 mm in dimension, that was attached to the left superolateral aspect of the uterus, inferior to the left cornu. It was fistulized to the mid-sigmoid colon. The sigmoid demonstrated diverticular disease with localized diverticulitis. There was no evidence of malignancy.
Discussion
Colo-uterine fistulas are rare, with the most common organs involved in colonic diverticular fistulas being the bladder (65%) followed by the vagina (25%) [4]. The uterine fundus serves as a protective factor against the development of colo-vaginal fistulas [5].
Aetiologies for colo-uterine fistula are various; in patients with uterine rupture [6], a loop of bowel can strangulate as it finds itself in the dehiscence, causing fistula formation as this becomes chronic, whereas in pelvic abscesses,6adhesions unite the colon and uterus to the abscess, creating a fistula. Other causes include radiotherapy [6], colorectal malignancy [6], uterine foreign bodies [6] and ectopic pregnancy [6]. In most cases, the fundus is involved [6]. In our patient’s setting of chronic inflammation, adherence of the colonic wall to the uterus ensued, leading to wall erosion, necrosis and fistula development [7].
The majority of presentations of colo-uterine fistulas include the presence of vaginal discharge and the expulsion of gas from the vagina [8]. Pelvic sepsis typically occur in acute presentations, and may be absent in those with chronic inflammation [8]. However, vaginal discharge was absent here, and lends credence to colo-uterine fistulas posing diagnostic dilemmas, as affirmed by Dadhwal et al. in 2008, who described a 24 year old with a colo-uterine fistula secondary to a uterine foreign body, in the absence of vaginal discharge and deranged laboratory results.
Imaging may pose difficulties in colo-uterine fistula diagnosis. In the literature, transvaginal pelvic ultrasound is the first-line modality of choice, however, it has low sensitivity and specificity in fistula detection [7]. In the emergency department, contrast enhanced CT Abdomen/Pelvis is of choice, given it is readily available [9], potentially revealing sigmoid diverticulitis, diverticular abscess, adherence between the sigmoid colon and uterus as well as air fluid levels in the uterus or in an adnexal mass [9]. Indeed, although CT holds low sensitivity for the visualization of a fistulous tract, the presence of intra-uterine air fluid levels should raise suspicion of a colo-uterine fistula. In addition, Perez et al. demonstrated the utility of CT with rectal contrast in visualizing the colo-uterine fistula [10]. In select cases, MRI Pelvis may be the most superior modality, as it is able to visualize the fistulous tract in T1 weighted images [11], in those where the colo-uterine fistula involves the rectum or anal sphincter, although in these patients chronic diverticulitis would not be the aetiology of such fistulas.
In our patient, TOA developed secondary to chronic sigmoid diverticulitis. TOA in the post-menopausal woman commonly develops in the setting of gynaecological malignancy or intra-uterine devices [12], and less in the presence of pelvic inflammatory disease (PID) or diverticulitis.
Treatment of colo-uterine fistula is surgical, with non-surgical options, such as percutaneous drainage or colonoscopic clipping of the fistulous tract, espoused for those with contra-indications for general anaesthesia [13]. The most commonly reported approach is en-bloc resection of both the uterus and affected colon, with an end-to-end anastomosis. In the setting of acute inflammation, a temporary defunctioning stoma is recommended [14]. In the woman of child-bearing age, it is recommended to perform uterine preserving surgery, as demonstrated by Kalaitsis et al. [15]
Declarations
Access to Open Access journal articles were facilitated by the University of Wollongong and Illawarra Shoalhaven Local Health District.
All authors are in agreeance with the contents of this article.
This article has not been published elsewhere.
Funding
No funding or financial support was utilized in producing this article.
Conflict of interest statement
None declared.
Consent to publish
Obtained from patient.
Ethics approval
Ethics approval was obtained by the Illawarra Shoalhaven Local Health District Ethics Committee.



