-
PDF
- Split View
-
Views
-
Cite
Cite
Andrej Nikolovski, Ivan Nevchev, Gligor Ristovski, Shqipe Misimi, Mare Burovska, Shenol Tahir, Metachronous colon cancer metastasis to abdominal wall 7 years after rectosigmoid resection: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad657, https://doi.org/10.1093/jscr/rjad657
Close - Share Icon Share
Abstract
Distant metastases from colorectal cancer to the abdominal wall are rare presentations of the end-stage of the disease. In this case, we present a female patient treated for Stage I rectosigmoid cancer with the late occurrence of abdominal wall metastasis, 7 years after the primary cancer surgery. The patient was treated with surgical excision and abdominal wall reconstruction with the use of synthetic mesh. Literature research on the abdominal wall recurrence/metastases from colorectal cancer was performed.
Introduction
Metachronous metastases from colorectal cancer (CRC) are well-known undesirable relapses of the primary tumor. They are expected to develop in ~70% of the patients treated with surgery alone or after conduction of the recommended oncologic multimodality regimens and are associated with poor prognosis [1]. Despite the most frequent metastasis sites such as the liver, lungs, and adrenal glands, unusual metastasis locations are reported [2]. One of the extremely rare is the abdominal wall. In some of the cases, the metastasis occurred several years after the index colorectal cancer surgery. We present such a case of late occurrence of abdominal wall metastasis originating from rectosigmoid cancer. Written informed consent was obtained from the patient.
Case report
A 73-year-old female patient was admitted to our hospital due to the existence of a tumor in the abdominal wall proved to be a metachronous adenocarcinoma metastasis. In October 2015, the patient was treated for rectosigmoid adenocarcinoma when rectosigmoid resection with primary anastomosis was performed. Pathology report revealed tumor stage I (pT2, pN0, pM0, pL0, pV0, pR0, G2, NG2). Only three lymph nodes were harvested and reported to be negative by the pathologist. Nevertheless, the oncologist decided not to initiate adjuvant chemotherapy, and recommendations for routine outpatient check-ups were advised. Two postoperative routine colonoscopies with normal findings were performed (in 2016 and 2022). Shortly after the second colonoscopy (in September 2022), elevated values of serum tumor markers were detected: Carcinoembryonic antigen (CEA) value of 15.2 ng/mL and Carbohydrate antigen (Ca) 19–9 value of 47.3 U/mL. The oncologist initiated adjuvant treatment with eight cycles of oxaliplatin and capecitabine. In March 2023, the additional elevation of markers followed (CEA value of 58.64 ng/mL, Ca 19-9 value of 665.12 U/mL, and Cancer antigen 15-3 value of 32.5 U/mL). In June 2023, serum marker levels decreased (CEA value of 35.5 ng/mL and Ca 19-9 value of 147 U/mL). Physical examination on routine follow-up revealed a palpable painless mass in the midline suprapubic region without skin involvement. Abdominal computerized tomography presented a solid tumor mass in the abdominal wall with dimensions of 70 × 40 × 80 mm and it was described as a suspected metastatic deposit by the radiologist (Figs 1 and 2). Core biopsy under ultrasonography guidance confirmed the presence of metastatic adenocarcinoma ˃7 years after the primary colon cancer surgery. A decision upon surgical removal was brought. The lesion was excised (Figs 3 and 4) and the defect of the abdominal wall was reconstructed by the use of composite mesh (Fig. 5). The postoperative course was uneventful and the duration of stay was 7 days. The pathology report confirmed the presence of metachronous metastasis from colon adenocarcinoma. Metastasis was measured to be 10 × 6 × 5 cm, completely occupied by a neoplastic infiltrate (Fig. 6). Immunohistochemistry staining showed positivity on Caudal-type homeobox 2 (CDX2) and Cytokeratin 20 (CK20) thus proving the origin of the metastatic deposit from colorectal adenocarcinoma (Fig. 7A–C).
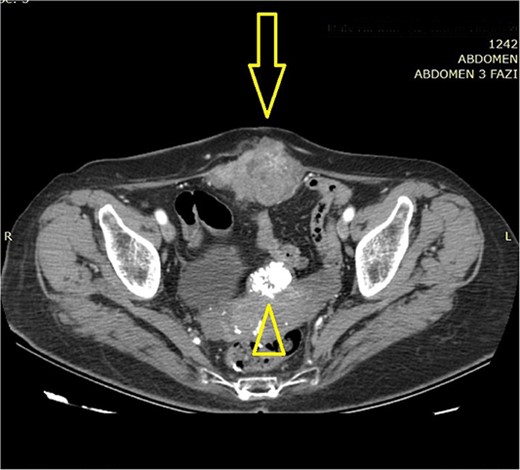
Abdominal computerized tomography (axial scan) shows a tumor in the abdominal wall (arrow) with the secondary finding of calcified uterine myoma (arrowhead).
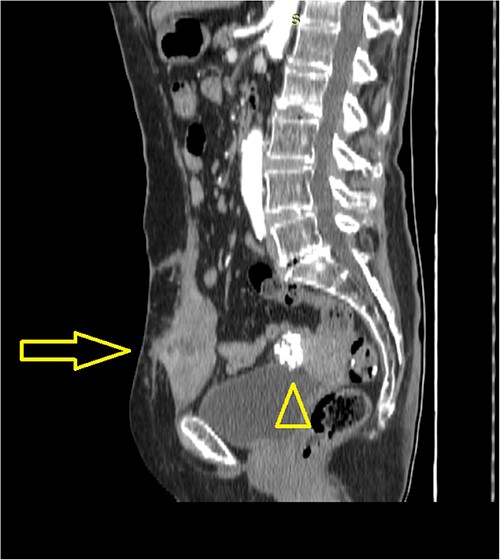
Abdominal computerized tomography (sagittal scan) shows a tumor in the abdominal wall (arrow) with the secondary finding of calcified uterine myoma (arrowhead).
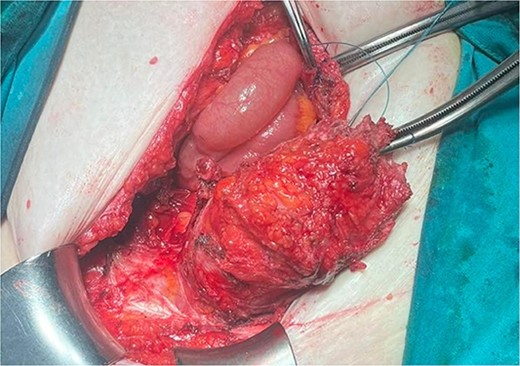
Intraoperative finding of the anterior wall metastasis during removal.


Abdominal wall defect reconstruction by the use of composite mesh.

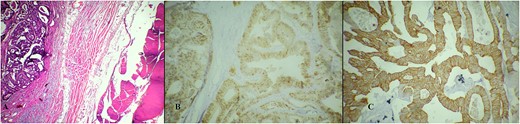
Microscopic pathology analysis of the metastasis. (A) Hematoxylin Eosin stain showing metastatic infiltrate of adenocarcinoma into soft tissue (abdominal wall muscle). (B) Immunohistochemistry stain showing positivity on CDX2. (C) Immunohistochemistry stain showing positivity on CK20.
Discussion
Metachronous solitary abdominal wall metastasis secondary to CRC is a rare end-stage presentation. It has been reported that it may occur via direct spread (invasion), by lymphatic and hematogenous routes, or by cancer cell implantation [3]. Skin and peristomal late recurrence are known and reported [4]. Nevertheless, the metastasis originated from the abdominal wall in this case, and no skin involvement or changes were present.
Thorough literature research by the use of keywords “colorectal cancer”, “metastasis”, “abdominal wall”, “recurrence”, and “metachronous” was performed. The reported rate of abdominal wall recurrence is 0.9% [5]. Metachronous abdominal wall metastases/recurrences have been reported previously and in general, rare case reports are present in the literature [6–11].
There seems no precise differentiation between the terms “abdominal wall metastasis” and “abdominal wall recurrence” in the literature. In one of the first series on the abdominal wall metastases from colorectal cancer of Ledesma et al., a total number of 22 patients were treated with surgery (part of them after failure with adjuvant radiotherapy or chemotherapy). The group was heterogeneous in terms of whether the abdominal wall metastasis was solitary or with concomitant intra-abdominal viscera involvement [12].
In the prospective multicentric study of Silecchia et al., out of 1565 patients, abdominal wall recurrence was reported in 13. The median time between the index surgery and the recurrence was 14.1 months [5].
Koea et al. points out that one should expect prolonged disease-free intervals in cases of solitary abdominal wall metastasis treated with curative surgical excision. In their series, almost half of the reported patients (31) had non-incisional site metastasis defined as recurrence separate from any pre-existing surgical incision or drain site. The time interval of the abdominal wall metastases occurrence was between 7 and 183 months [13].
The current series and case reports include patients with different stages of the disease and cannot explain the mechanism of abdominal wall metastasis occurrence. This especially refers to patients with postoperative early stage colorectal cancer and negative lymph node status. This may be partially explained by the insufficient number of harvested lymph nodes during the index surgery and the inadequate postoperative cancer staging [8]. In this report, the postoperative stage is also questionable due to the insufficient number of detected and analyzed lymph nodes.
Attempts for oncologic treatment of the abdominal wall metastases resulted in unfavorable outcomes and clinically uncontrolled progression. In the series of Ledesma, part of the patients received radiation therapy (average of 4000 radiations absorbed doses), and to others, systemic chemotherapy 5-fluorouracil (5-FU 500 mg/m2) was given. Subsequently, the patients were subsided to surgery [12]. The general conclusion was that surgery for localized solitary abdominal wall metastasis should be the preferred treatment [12, 13].
This report presents the late occurrence of CRC metastasis to a rare location (abdominal wall) in a patient with early stage rectosigmoid cancer successfully treated with surgery and abdominal wall reconstruction.
Conflict of interest statement
None declared.
Funding
None declared.



