-
PDF
- Split View
-
Views
-
Cite
Cite
Geraint Berger, Daniel French, Palliative management of a malignant tracheoesophageal fistula using repeat endobronchial laser debridement and esophageal stenting, Journal of Surgical Case Reports, Volume 2023, Issue 12, December 2023, rjad590, https://doi.org/10.1093/jscr/rjad590
Close - Share Icon Share
Abstract
A 71-year-old female presented with progressive dysphagia and unexplained weight loss. Computed tomography and esophagogastroduodenoscopy (EGD) revealed invasive esophageal squamous cell carcinoma, which was initially treated with local radiation and esophageal stenting. Over the next year, the patient experienced multiple symptoms and hospital admissions consistent with a malignant tracheoesophageal fistula, despite negative findings on imaging, bronchoscopy, and EGD. Prophylactic antibiotics were initiated based on symptomatology to prevent septic episodes. Stent erosion into the membranous trachea was eventually observed. Neodymium-yttrium-aluminum-garnet laser bronchoscopy was used periodically to debulk the invading tumor around the stent. A percutaneous endoscopic gastrostomy tube was also inserted to facilitate enteral nutrition and avoid aspiration pneumonia. The patient reported significant improvements in respiratory symptoms following each laser debridement and has progressed well beyond the life expectancy associated with malignant tracheoesophageal fistula.
Introduction
Malignant tracheoesophageal fistula (TEF) is a life-threatening complication of esophageal cancer resulting in a communication between the respiratory tract and the esophagus. Given the proximity of the trachea and proximal left mainstem bronchus to the esophagus, tumors originating in the esophagus can readily invade the membranous portion of the airway [1]. Approximately 5%–10% of patients with primary esophageal cancer develop TEF [2]. TEF is significantly more common in patients with squamous cell carcinoma (SCC) and locally advanced mid-esophageal involvement [3]. T4 and N3 stage disease, radiotherapy, stenosis, and large tumor thickness have also been identified as risk factors for fistula formation [4]. Patients with advanced disease involving the airway have significantly higher morbidity and mortality, attributable to frequent aspiration pneumonia and airway obstructions [5].
Unfortunately, there is little evidence to guide the management of patients with airway involvement secondary to invasive esophageal cancer [3]. We present a patient with a TEF secondary to esophageal SCC managed with palliative repeat laser bronchoscopy for respiratory symptom control achieving significant improvement in symptoms and quality of life. She is alive 24 months after presentation, well beyond her anticipated life expectancy.
Case report
A 71-year-old female presented in May 2020 with a 6-month history of progressive dysphagia and weight loss. Her past medical history was significant for recurrent ductal carcinoma in situ of the left breast. She was a never smoker. Esophagogastroduodenoscopy (EGD) showed a proximal circumferential mass with friable mucosa and ulcerations at 15 cm (Fig. 1A–D). Computed tomography (CT) imaging showed significant soft tissue thickening and luminal narrowing of the esophagus from the sternoclavicular joints to the carina (Fig. 2E). An esophageal stent was placed to support nutrition, which improved the patient’s dysphagia. Biopsy confirmed invasive SCC. Subsequent positron emission tomography imaging revealed 18-fluorodeoxyglucose-avid mediastinal, bilateral supraclavicular, and subdiaphragmatic lymph nodes. Bronchoscopy showed no evidence of tumor invasion into the airway.
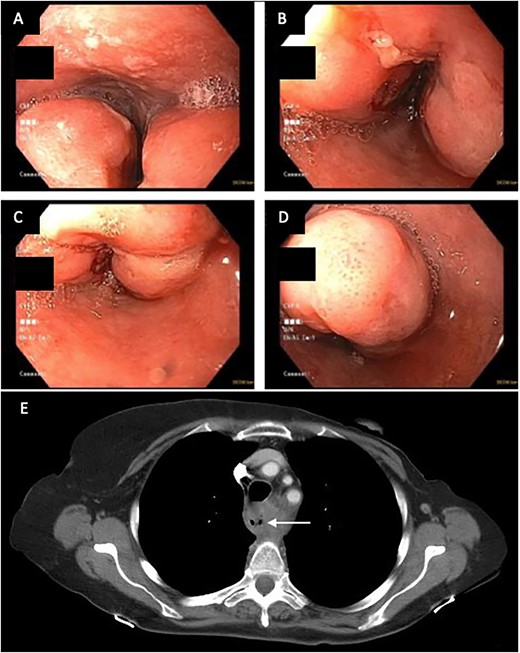
(A–D) EDG images showing circumferential esophageal mass with friable mucosa and ulcerations. (E) CT chest showing marked soft tissue thickening with luminal narrowing in the upper esophagus, which extended to a level below the carina.
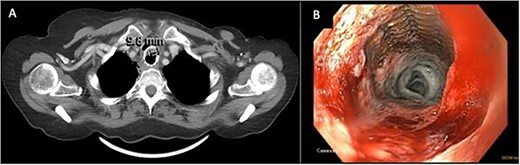
(A) CT image from January 2021 showing severe narrowing of the lumen of the esophagus proximal to the stent. (B) EDG from February2021 showing response to balloon dilation of a stricture proximal to the indwelling stent.
Initial treatment with 30 Gy of radiation significantly reduced metastatic lymph node burden in the mediastinal and supraclavicular nodes. The patient’s energy and appetite improved significantly, and adjuvant chemotherapy was aborted because there was no measurable disease on follow-up CT.
The patient re-presented in November 2020 with a persistent cough, dyspnea, and vomiting. Repeat CT revealed an interval increase in the esophageal mass causing complete stent occlusion and extrinsic compression of the posterior trachea. Bronchoscopy confirmed trachea compression, with nodular granulation tissue seen invading the mid-trachea. The lower airways appeared grossly contaminated. Based on these bronchoscopic findings, evidence of disease progression, and clinical presentation, a provisional diagnosis of a TEF was made. Despite a biopsy showing only granulation tissue, there was concern for recurrent disease based on CT imaging, therefore an additional 18 Gy of radiation was delivered.
Palliative supports for the patient were arranged. CT scan at this time (January 2021, Fig. 2A) showed severe luminal narrowing of the esophagus proximal to the stent. The patient initially declined a feeding gastrostomy tube to avoid further aspiration. Instead, repeat EGD with balloon dilatations were performed to relieve dysphagia (Fig. 2B). TEF was still not detected on bronchoscopy or on barium esophagogram. The patient continued to have recurrent pulmonary infections treated with oral antibiotics. In April 2021, a percutaneous endoscopic gastrostomy tube was inserted to facilitate enteral nutrition and minimize aspiration.
In April of 2022, the patient developed recurrent pneumonias, hemoptysis, and progressive dyspnea, raising concern of tumor invasion into the airway. Bronchoscopy confirmed a large tumor encompassing 2/3 of the airway, with evidence of stent erosion through the trachea (August 2022, Fig. 3). Laser debridement of the tumor was successfully performed.

Bronchoscopic evidence of tumor growth into the trachea with evidence of stent erosion (August 2022).
This was the first clear evidence of esophagotracheal communication. Laser debridement was successfully performed again in November 2022, leaving only a small portion where the stent eroded the trachea. On post-bronchoscopy Day 3, the patient reported significant improvements in breathing and energy. Over 6 months, she underwent laser debulking of the tracheal mass twice to manage tumor ingrowth (January and April 2023). Debridement was performed each time using a neodymium-yttrium-aluminum-garnet laser (Fig. 4). Between 380 and 560 joules were delivered to cauterize and debulk the invading tumor. The patient continues to be followed for palliative tumor debulking for ongoing symptom management.

Bronchoscopic view of the endobronchial obstruction. Invasion of the esophageal malignancy can be seen, as well as erosion of the esophageal stent into the lumen of the trachea.
Discussion
The management of malignant TEF remains a significant challenge. Without prompt intervention, survival time is measured in weeks to months, with the cause of death most often attributed to aspiration pneumonia or pulmonary sepsis [6]. Despite inconclusive radiographic and bronchoscopic evidence, the patient was treated early for a presumed TEF based on symptomatology and responded well to palliative management.
As many patients with TEF are poor surgical candidates, an endoscopic approach is often taken to management. Esophageal stenting provides symptom improvement and significantly prolong life in patients with malignant TEF [3, 7]. However, caution should be taken in patients receiving chemo- or radiotherapy, as tumor necrosis can increase risk of fistula formation [4, 8]. These patients should be closely monitored for respiratory tract complications. In this case, despite numerous repeat investigations for a TEF, all results including barium esophagography were negative. Novel techniques have been developed in recent years to help diagnose inconspicuous TEF, including the use of capnography during esophagoscopy with CO2 insufflation [9]. This report emphasizes on the importance of early intervention if clinical suspicion of TEF is high, and close monitoring in patients undergoing cancer treatment, especially within the first 3–6 months.
Interventional bronchoscopy plays a critical role in the treatment and palliation of malignant airway obstructions [10]. Bronchoscopic laser therapy is a thermal ablation technique with cutting and coagulation capabilities, making it highly useful for treating intraluminal obstructions [11]. Advantages include its rapidity, repeatability, compatibility with concurrent therapies [12], and ability to regain airway patency [13]. It has been shown to increase survival in cases involving malignant airway obstructions, providing symptom relief, and allowing for increased duration of adjuvant therapy [14, 15]. We report on the use of bronchoscopic laser debulking of an invasive esophageal tumor for palliative symptom management for a malignant TEF. The patient-reported improvement in dyspnea and an overall increase in quality of life, well beyond her anticipated life expectancy.
Conflict of interest statement
None declared.
Funding
None declared.
References
- stents
- antibiotic prophylaxis
- computed tomography
- weight reduction
- aspiration pneumonia
- debridement
- deglutition disorders
- upper gastrointestinal endoscopy
- enteral nutrition
- bronchoscopy
- lasers
- life expectancy
- tissue membrane
- neodymium
- signs and symptoms, respiratory
- tracheoesophageal fistula
- yttrium
- aluminum
- diagnostic imaging
- neoplasms
- palliative care
- trachea
- squamous cell carcinoma, esophageal
- gastrostomy tubes
- hospital admission
- erosion
- laser bronchoscopy



