-
PDF
- Split View
-
Views
-
Cite
Cite
Alberto de Castro Pochini, Benno Ejnisman, Carlos V Andreoli, Paulo H S Lara, Leandro M Ribeiro, Moises Cohen, Paulo S Belangero, Debora C Hipolide, Rupture of the bilateral and simultaneous tendon of the pectoralis major muscle. Description of three cases, Journal of Surgical Case Reports, Volume 2023, Issue 11, November 2023, rjad531, https://doi.org/10.1093/jscr/rjad531
Close - Share Icon Share
Abstract
Pectoralis major muscle tendon ruptures associated with physical activity or effort are no longer uncommon in the medical literature. Treatment has also evolved significantly in the last 20 years. However, simultaneous bilateral rupture has only been described in a few cases. This article reports three cases with simultaneous bilateral rupture and describes the examinations and treatment performed. Bilateral lesions, although infrequent, also require early diagnosis and treatment in the acute phase. The chronic phase requires tendon grafting for full correction and a slow rehabilitation process.
Introduction
Descriptions of cases of rupture of the pectoralis major muscle (PMM) tendon are no longer uncommon in the literature [1–3], including videos [4] in competitions etc. However, bilateral and simultaneous cases are still rare [5–7]. Generally, they are related to weightlifting but not always. We present three cases of bilateral rupture of the pectoralis major tendon. Two related to weightlifting and one not related to weightlifting but to sudden strain of the PMM and rupture. Always perform a differential diagnosis with Poland’s Syndrome (bilateral pectoralis major agenesis) [8].
Case reports
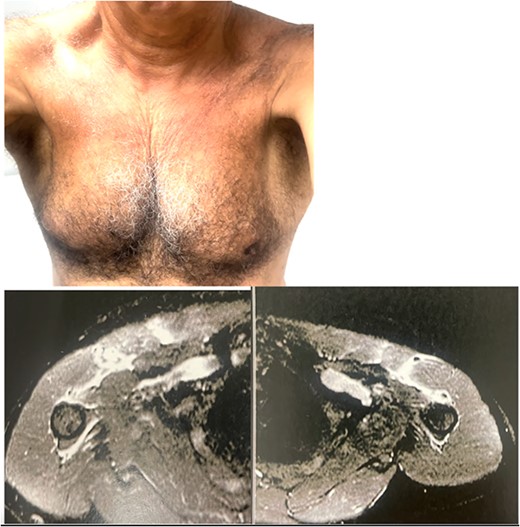
Case 1: a 25-year-old patient (Figs 1 and 2), weightlifter and physical education teacher, denied the use of anabolic steroids, performing supine exercises weighing 100 kg, felt crunch and bilateral functional loss. Both surgeries were performed at the chronic stage (after 1 month), one with 1 year and the other with 1.6 years, both using fascia lata graft (Fig. 2). Returned to weight training, right side with some aesthetic deformity and left side with improved strength and aesthetics.
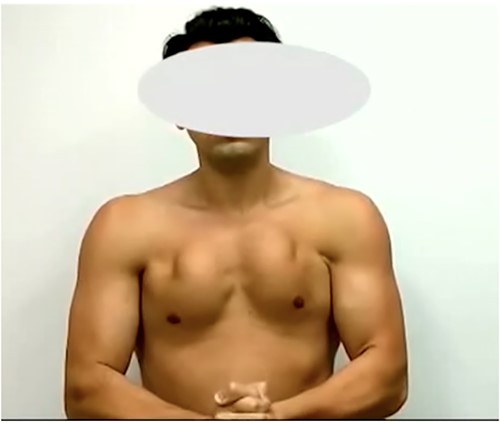
Patient with clinical examination of significant retraction of the PMM with lesion in chronic stage.
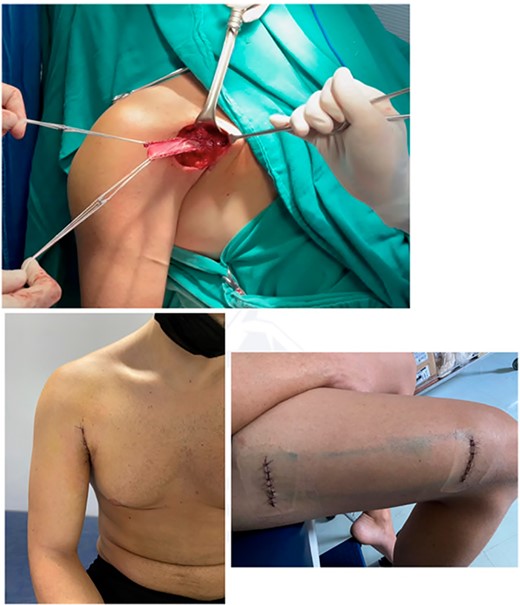
Surgical images showing the intraoperative fascia lata graft, cosmetic aspect of the axillary surgical incision and thigh incision for removal of 20 cm of autologous fascia lata graft.
Case 2: a 29-year-old bodybuilder lifting 250 kg supine weight suffered simultaneous bilateral rupture of the pectoralis major tendon 3 months ago (Figs 3 and 4). Reports use of anabolic steroids associated with the time of the rupture. A tendon reconstruction was performed 5 months after the injury using fascia lata graft (Fig. 5).

Clinical examination of a patient with simultaneous bilateral pectoralis major rupture in a supine press exercise with a 240 kg load.
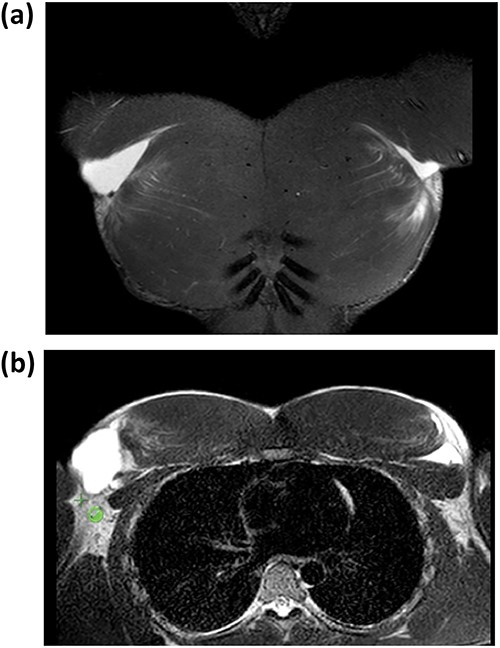
Coronal and axial T2-weighted MRI images showing rupture of the tendon of the bilateral PMM.
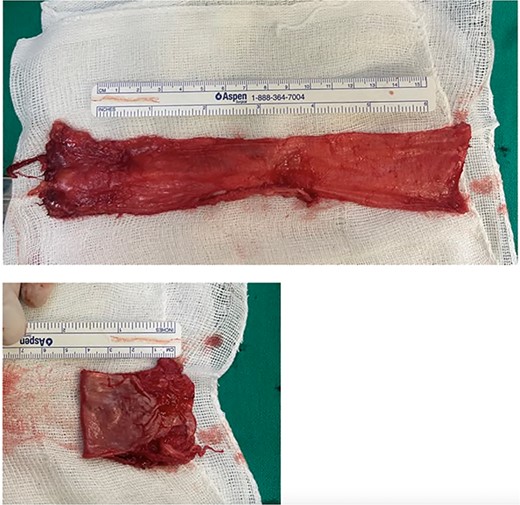
20 cm autologous folded fascia lata graft aimed at PMM tendon reconstruction.
Case 3: patient (Fig. 6) 64 years old, active, ex-competitive tennis athlete, and multiple sports enthusiast. When descending into the pool, he made a sudden effort to raise his trunk causing a bilateral rupture of the pectoralis major tendon. Reports significant loss of strength for general physical activity after 6 months. Opted for conservative treatment.
Patient 3 with PMM tendon rupture after sudden force to climb a pit with both hands and exerting great effort to adduct the shoulder.
Discussion
Injuries to the tendon of the PMM are not so frequent in orthopaedic emergency care; however, with the growth of bodybuilding gyms and the use of anabolic steroids [1, 3, 4] there has been a significant increase in the number of cases that end up seeking medical attention, either in the acute phase due to pain and associated ecchymosis in the arm region or in the chronic phase due to alteration in loss of strength and axillary deformity (cases 1, 2, and 3). Two of the patients described had suffered weightlifting injuries and only one of them (case 2) reported use of anabolic steroids. Case 3, who suffered rupture due to intense and abrupt shoulder exertion, denied steroid use and it did not occur during weight training exercises.
It is very important to consider the importance of early diagnosis of PMM tendon rupture (with ecchymosis and loss of S sign) [9] or axillary wall alteration [2, 3]. In these cases, the lesion presents an important loss of strength and deformity that, in young or active patients who practice physical activity, indicates surgical treatment to repair the lesion within 30 days [2, 3, 9, 10]. After 30 days the need for tendon reconstruction with autologous graft or allograft has to be considered, grafts can be semitendinosus and gracilis, achilles, fascia lata [2, 3, 11–14]. In bodybuilding patients in whom the injury occurs in bench press associated with heavy loads and the use of anabolic steroids, consider the need for grafting (reconstruction) even in acute cases, as in some cases there is a complex injury with great retraction, which makes repair unfeasible even in the acute phase [12–14].
The use of grafts contributes greatly to a better biological site for reinsertion or reconstruction. The fascia lata has already been used by our group in several cases with follow-up after 2 years with good functional results (Bak’s criterion) [2, 3, 15].
Bak’s Criterion [15]:
Excellent: no symptoms, normal range of motion, no cosmetic changes, no adductor weakness, able to return to sports activities.
Good: below normal range of motion, no cosmetic modifications
20% isokinetic peak of torque deficit.
Fair: limited range of motion, unable to return to sports activities, poor cosmetic status.
Bad: continuous pain, requiring surgical revision.
Patients 1 and 2 had an excellent functional result and Patient 3 had a reasonable functional result. In the use of the fascia lata graft, the removal is performed with two transversal incisions and in general the patient reports little pain post-operatively, leading some patients to a more intense dislocation (16).
In general, we use buttons with an adjustment as it is a deep entry. The use of anchors is not always possible because at some point of the bone fixation the humerus is still medullary and the anchor can stay in the medullary bone compromising the fixation. In these patients, the 2 operated on underwent reconstruction using fascia lata graft and adjustment buttons. If the early diagnosis and treatment had been done, perhaps the surgical repair of the tendon with the bone could have been performed with cortical buttons, with a faster healing evolution, since in the repair the healing occurs between the PMM and the humerus of the patient. In the reconstruction performed in chronic cases, there is a need for cellularization of the graft, either autologous or from a tissue bank, for healing between the muscle tendon and tendon-bone interface. Rehabilitation also for passive motion gain begins after 4 weeks for repair and 6 to 8 weeks for reconstruction. The three patients in the article came to us after 1 month of injury. In general, the treatment is performed unilaterally to ensure greater comfort in the patient’s post-operative period and a good functional result.
As the cases presented in this article are bilateral, it is not possible to compare the two sides, making the isokinetic evaluation difficult. The rehabilitation of these cases generally begins with physiotherapy and the gaining of range of movement starting within 4 weeks. In the case of the use of a graft, gain of range of movement starts between 6 and 8 weeks. A stiff shoulder is not expected after PMM tendon rupture because the surgery is extra-articular and so does not involve problems of arthrofibrosis.
Conclusion
PMM tendon rupture is not a very common injury and bilateral simultaneous rupture is even more uncommon but can also occur as described in these cases.
Conflict of interest statement
None declared.
Funding
This work had the support of the state government FAPESP – PROCESS NUMBER 2014/04180-6 to carry out the magnetic resonance exams. Because Brazil is the second country in the world in gym and crossfit practitioners, the injury of the pectoralis major has increased and its association with anabolic steroids has concerned those responsible for public health.



