-
PDF
- Split View
-
Views
-
Cite
Cite
Ryotaro Urabe, Makoto Miyamae, Yoshiki Minegishi, Kunihiro Nakai, Surgical treatment for a giant venous malformation of the parotid area, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad591, https://doi.org/10.1093/jscr/rjad591
Close - Share Icon Share
Abstract
This report discusses the surgical treatment of a giant parotid venous malformation (VM) that had grown beyond the dimensions of the parotid gland, causing significant displacement. Special attention was paid to identifying the facial nerve, which was found to traverse the surface of the VM. Although, in our case, the facial nerve ran superficially on the VM, it is possible that a portion of it penetrated the mass. A two-stage excision and revision surgery strategy was employed due to the complexity of assessing deformities after removing the giant lesion. During the initial surgery, the displaced superficial lobe of the parotid gland was repositioned to its original location and carefully laid over the facial nerve, ensuring its safety during the subsequent procedure.
Introduction
Parotid gland venous malformations (VMs) are rare, comprising a small fraction of parotid tumors. Achache et al. conducted a 10-year survey, reporting a 1.6% incidence rate with 60% in the superficial lobe, 20% in the deep lobe, and 20% in the masseter muscle [1]. Beahrs et al. reported a rate of 0.53% and a lesion size of 2–5 cm [2]. Primary treatment options for VMs include surgical intervention and sclerotherapy [3], depending on the lesion’s condition. In parotid VM cases, preserving the facial nerve is crucial to avoid complications [3].
This report details the surgical management of an oversized parotid VM.
Case report
A 16-year-old girl presented with a long-standing right parotid mass that had progressively enlarged since childhood. A biopsy at age 13 confirmed it as a VM.
Examination revealed a 10 cm × 6 cm subcutaneous mass in the right parotid area (Fig. 1a), causing facial contour asymmetry. Notably, there was no facial nerve paralysis.
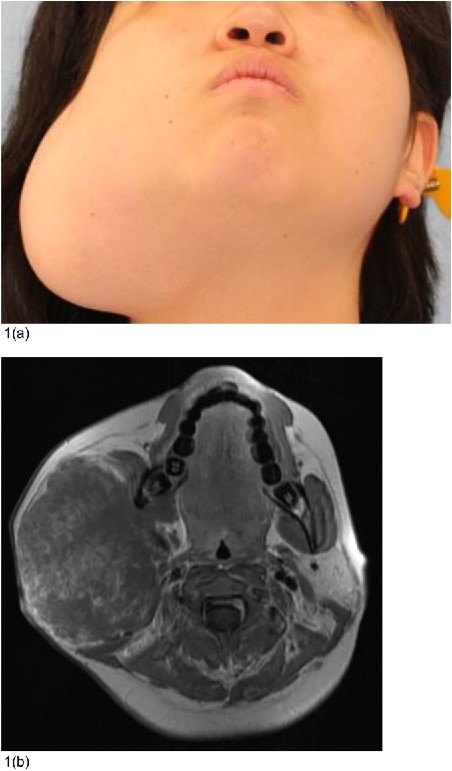
Preoperative condition. (a) A 16-year-old woman had a subcutaneous mass measuring 10 × 6 cm in the right parotid area. Her facial contours were asymmetrical. (b) MRI images displayed a 75 mm × 97 mm × 87 mm lobulated mass with heterogeneous internal contrast.
Magnetic resonance imaging (MRI) displayed a 75 mm × 97 mm × 87 mm lobulated mass with heterogeneous internal contrast, indicating a low-flow VM.
Given the considerable size and complexity of the VM, a two-stage excision and revision surgery approach was planned.
First surgery
During the initial surgery, the patient underwent an excision of the VM in the right parotid area, following a similar approach to parotidectomy. An S-shaped skin incision was made from the front of the ear to the mandible, and subcutaneous dissection was performed along the surface of the mass. The marginal mandibular branch of the facial nerve was identified on the surface of the mass at the mandibular area (Fig. 2a).
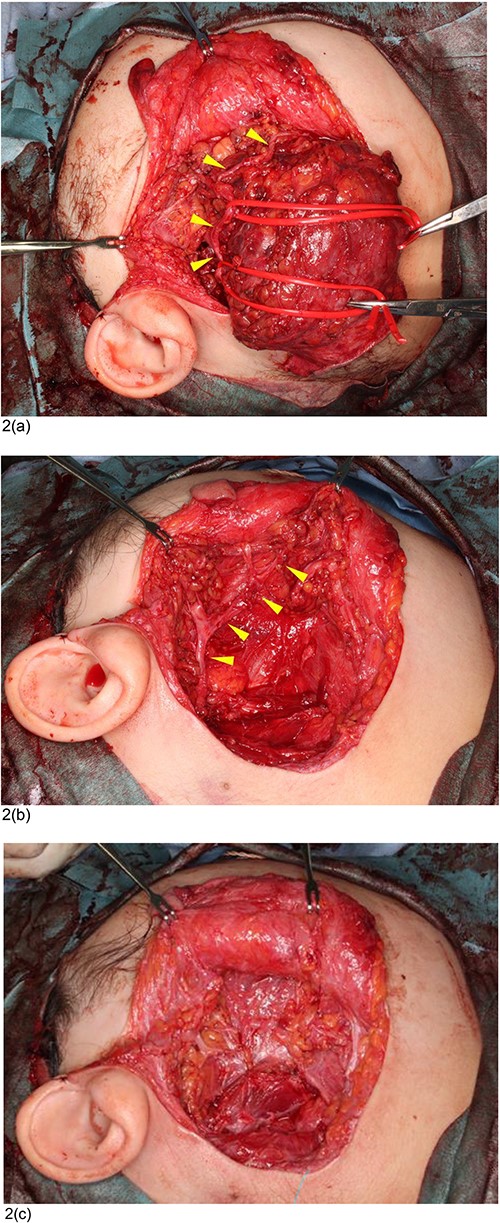
Intraoperative condition at the first surgery. (a) The marginal mandibular branch of the facial nerve (triangles) was identified on the surface of the mass at the mandibular area. (b) The facial nerve (triangles) was preserved after excision of the parotid VM. (c) The displaced superficial lobe of the parotid gland was repositioned to its original location and laid over the facial nerve.
Dissection progressed proximally between the facial nerve and the mass, with the facial nerve successfully preserved (Fig. 2b).
Blood vessels entering the mass were ligated and cut, and the mass was completely excised.
Although the mass had initially been located in the deep lobe of the parotid gland, its growth had led it to the superficial layer. During the surgery, the displaced superficial lobe of the parotid gland was repositioned to its original location and laid over the facial nerve (Fig. 2c).
The excised mass measured 9 × 8 cm. The lumen was spongy. Histopathological examination revealed VM.
Second surgery
Two years after the first surgery, a concave deformity measuring 7.5 × 5 cm was observed in the right parotid area (Fig. 3).
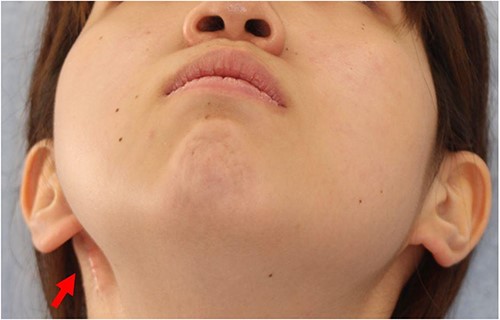
Postoperative condition 2 years after the first surgery. A concave deformity (arrow) was observed in the right parotid area.
A skin incision was made along the previous incision and the concave, deformed area was dissected on the superficial lobe of the parotid gland (Fig. 4a).
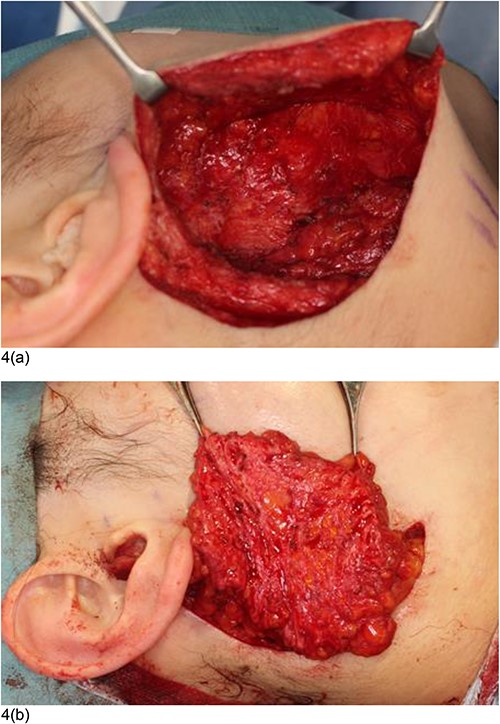
Intraoperative condition at the second surgery. (a) The concave, deformed area was dissected on the superficial lobe of the parotid gland. The facial nerve was not exposed, and injury to the facial nerve was safely avoided. (b) The flap was filled and firmly fixed into the concave deformity area.
The facial nerve was not exposed, ensuring its safety throughout the procedure. A 12.5 × 7.5 cm free groin flap was harvested from the right groin area. The superficial circumflex iliac artery and superficial circumflex iliac vein, responsible for supplying blood in the flap, were anastomosed to the lingual artery and superior thyroid veins. The flap’s skin was removed, and the dermal surface was placed over the upper surface of the defect. The flap was secured in place, correcting the concave deformity (Fig. 4b).
Six years following the second surgery, the concave deformity had significantly improved, restoring symmetrical facial contours (Fig. 5a).
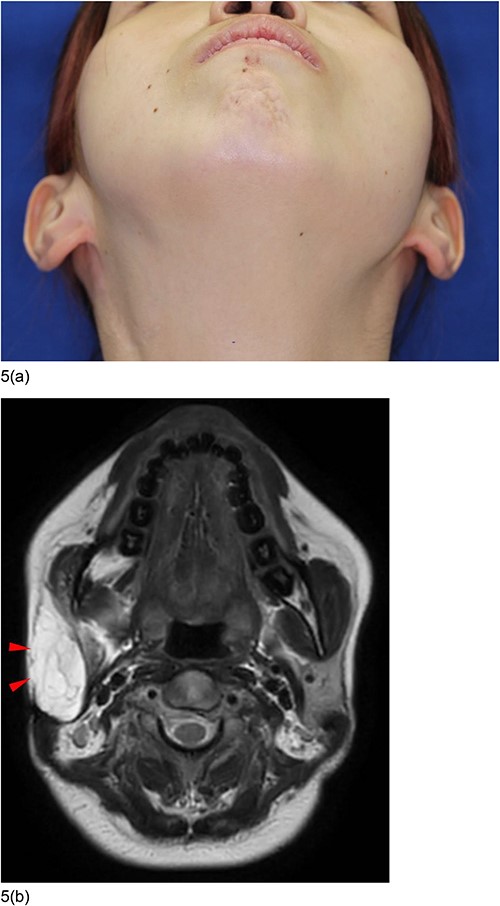
Postoperative condition 6 years after the second surgery. (a) The concave deformity was improved and the facial contours became symmetrical. (b) MRI images showed that the concave deformed area was filled with fat of the flap (triangles).
Notably, there were no complications such as facial nerve paralysis or Frey syndrome. MRI showed that the concave, deformed area was filled with fat from the flap (Fig. 5b).
Discussion
This case highlights the unique challenge posed by a giant parotid VM that had grown larger than the parotid gland. As the VM expanded, it displaced the superficial lobe, deep lobe, and lower pole of the parotid gland, complicating the surgical approach. The facial nerve is believed to traverse the VM surface. The usual anatomical markings for parotidectomy are not helpful [4–6], and meticulous identification of the facial nerve on the VM’s surface is imperative. In this case, the facial nerve was observed to pass through the VM’s surface, although the MRI had a lobulated mass, raising the possibility that a segment of the facial nerve might have penetrated the mass.
Given the complexities involved, a two-stage excision and revision surgery was planned because it was difficult to evaluate the deformity after the excision of the giant mass. The objective was to safeguard the facial nerve during the second surgery. To achieve this, the displaced superficial lobe of the parotid gland was repositioned to its original position and carefully positioned over the facial nerve, preventing potential nerve injury during the subsequent procedure. This surgical technique also served to mitigate the risk of Frey syndrome.
The concave deformity observed post-VM excision was attributed to mandibular hypoplasia resulting from the presence of the giant VM during childhood. Thus, reconstruction was performed using a free groin flap, aligning with principles applied in cases of hemifacial microsomia and facial lipodystrophy [7–9]. Previous studies have indicated that preventing postoperative flap drooping caused by gravity can be achieved by positioning the dermal surface of the groin flap in contact with the lower surface of the defect [7–9]. However, in our case, we opted to place the flap’s dermal surface on the defect’s upper surface. This decision was influenced by the potential to achieve a more accurate replication of the contours of the mandibular ramus and angle. No postoperative flap drooping was observed. Several factors contributed to this successful outcome, including the well-developed surgical field and secure fixation of the flap. In addition, this approach may have reduced the concave deformity toward the lateral side of the cheek, in contrast to hemifacial microsomia and facial lipodystrophy.
In conclusion, this report details the successful surgical excision of a giant parotid VM that had grown beyond the dimensions of the parotid gland. Preserving the facial nerve was paramount, and careful identification of the nerve on the VM’s surface ensured its safety. The innovative approach of using the displaced parotid gland during the first surgery to shield the facial nerve from harm during the second surgery resulted in the effective reconstruction of the concave deformity following VM excision.
Conflict of interest statement
None declared.
Funding
None declared.



