-
PDF
- Split View
-
Views
-
Cite
Cite
Mathew C Moolamannil, Hanad Ahmed, Gertrud Devecseri, Yogeshkumar Malam, Max Wilde, Dipankar Chattopadhyay, Two cases of Rapunzel syndrome in adult males, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad571, https://doi.org/10.1093/jscr/rjad571
Close - Share Icon Share
Abstract
Trichobezoar are foreign bodies formed from undigested hairs that accumulate in the gastrointestinal tract and cause obstruction. Trichobezoar are usually found in the stomach but when the tail of the bezoar extends into the small intestine it is referred to as Rapunzel syndrome. Patients are usually females and have a history of psychiatric illness. However, in this study, we present two cases of Rapunzel syndrome in adult male patients that were managed with surgery. Trichobezoar should be considered in all patients with a history of psychiatric illness presenting with abdominal symptoms regardless of gender.
Introduction
Trichobezoar are foreign bodies consisting of undigested hair fibres which are ingested by patients (trichophagia) [1]. Typically trichobezoars accumulate in the stomach, but when extending into the small bowel these cases are referred to as Rapunzel syndrome [2].
Trichobezoar and Rapunzel syndrome are usually seen in children and young females with a range of psychiatric conditions such as schizophrenia, post traumatic stress disorder, attention deficit hyperactivity disorder, and depression.
Adult males have rarely been reported in the literature. Here we present two cases of Rapunzel syndrome in young men with psychiatric disease.
Case reports
First case
A 24-year-old male presented to the emergency department with a 4-week history of progressive upper abdominal pain and vomiting with weight loss, decreased appetite, and early satiety. No other significant past medical history was offered by the patient.
On examination, his vital signs were stable with a blood pressure of 120/76 mmHg and pulse of 97 beats per minute. Abdominal examination revealed tenderness in the epigastrium with no palpable mass. Bloods showed an elevated white cell count of 15.6 × 109 cells/μl and a C- Reactive Protein (CRP) of 30 mg/L with normal renal function.
A CT scan of the abdomen and pelvis was performed showing multiple large foreign bodies in the stomach and proximal small bowel (as seen in Fig. 1), with a differential diagnosis of bezoars. Given these findings, the history was revisited and the patient was asked if he had consumed anything unusual. The patient admitted to habitually consuming his own hair as a response to stress for at least 20 years prior to presentation.
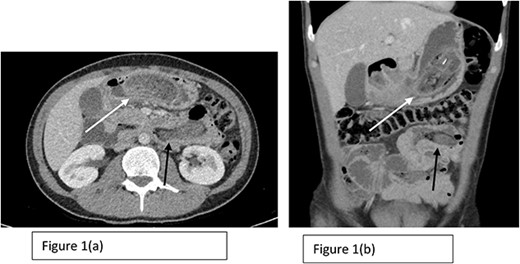
Axial (a) and coronal (b) sections of CT scan showing the presence of Trichobezoar in the stomach with extension into the small bowel (The white arrow in both Fig. 1a and b shows the trichobezoar in the stomach while the back arrow shows the extension into the small bowel with surrounding inflammation).
The patient underwent a gastroscopy which confirmed a large trichobezoar in the stomach with a tail extending into the duodenum (as seen in Fig. 2) and subsequently underwent laparoscopic gastrotomy for the removal of the trichobezoars. Laparoscopically an incision in the anterior wall of the stomach was performed and both trichobezoars were manipulated and delivered through the same gastrotomy (as seen in Fig. 3).
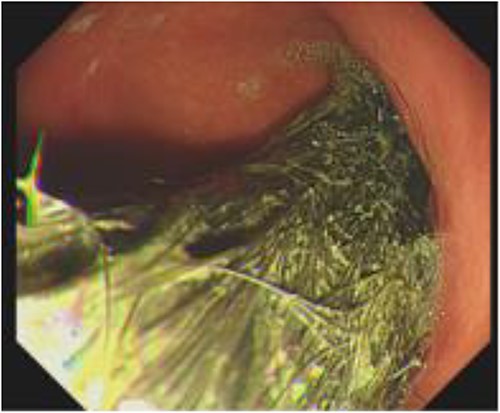
Gastroscopy image showing the presence of hair fibres forming the trichobezoar in the stomach.

Trichobezoar specimen removed intact showing the outline of the stomach and extension into the small bowel.
Postoperative recovery was complicated by pleural effusion, pneumonia, and pulmonary embolism. The patient was reviewed by the psychiatric service and formally diagnosed with depression and anxiety and started on sertraline 50 mg. The patient was discharged home on postoperative Day 29.
Second case
A 28-year-old male presented to the Emergency Department with a 1-week history of severe vomiting and dehydration. The previous history was significant for a 2.5-year history of weight loss for which the patient had presented to various healthcare settings previously. The patient had a diagnosis of Asperger’s syndrome.
On examination, there was a palpable mass in the epigastrium, but no tenderness or distension. The patient appeared clinically dehydrated. Laboratory findings included creatinine 270 μmol/L, urea 23.5 mmol/L, sodium 123 mmol/L, white cell count 24.5 × 109/μl, and C-reactive protein 5.4 mg/L.
A computed tomography scan of the abdomen and pelvis showed a significantly distended stomach, duodenum, and proximal jejunum, with a large bezoar seen intraluminally (demonstrated in Fig. 4).
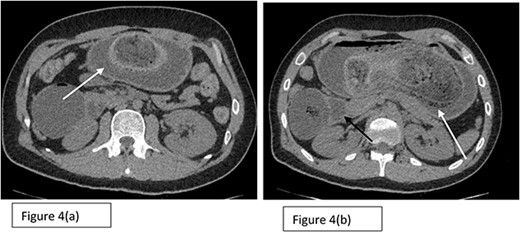
Axial sections (a) and (b) of CT scan showing the presence of Trichobezoar in the stomach (white arrows) with extension into the duodenum noted as well.
The patient underwent a midline laparotomy, gastrotomy, and enterotomy to remove the trichobezoars from the stomach and duodenum and recovered well postoperatively (as seen in Fig. 5).

Discussion
Rapunzel Syndrome is a rare complication where trichobezoars cross the pylorus to enter the small bowel. Typical patients are children and young females with a history of psychiatric illness. First described by Vaughan et al. in 1968 [3], the eponymous Rapunzel Syndrome is named after the long haired female character in the fairy tale written by the Grimm Brothers in 1812. We report a series of two male patients with Rapunzel syndrome. Both patients ultimately had an underlying diagnosis of psychiatric illness which is a risk factor for trichophagia, and it is interesting to note both male patients had long hair.
The presentation of trichobezoars is often non-specific and given its rarity making a diagnosis is challenging. Symptoms include abdominal pain and vomiting and an abdominal mass may be palpable. Emergency presentations with complications such as obstruction, peritonitis or perforation can also occur [4, 5].
Diagnosis is aided with cross sectional imaging such as CT scanning. The confirmation of the diagnosis of trichobezoar/Rapunzel Syndrome is often established only by reviewing imaging and revisiting the history with the patient [6]. Diagnosis is often delayed as patients do not readily admit to ingesting hair or other inorganic material and direct questioning is often useful to establish the history.
Therefore a high index of suspicion is required when evaluating patients presenting with long standing abdominal complaints and a background of psychiatric illness.
Traditionally laparotomy was the approach of choice to remove the trichobezoar, but modern management options include endoscopic removal and laparoscopic surgery. In a retrospective review of 108 cases of trichobezoar by Gorter et al., it was noted that only 5% of attempted endoscopic removals were successful (small trichobezoars may respond to endoscopic fragmentation and vigorous lavage) and 75% of attempted laparoscopic surgical extractions were successful. In cases were a laparoscopic approach failed, laparotomy was performed.
In addition to acute surgical treatment, psychiatric consultation is necessary to treat any underlying psychiatric illness which may be driving behaviours such as trichotillomania and trichophagia in order to prevent relapses [7].
Conclusion
Trichobezoar and Rapunzel Syndrome are a rare cause of abdominal pain and obstruction, usually with a protracted and vague presentation. Typical patients are children and females with a history of psychiatric illness, but our report demonstrates that male patients with an underlying psychiatric diagnosis are also at risk. A high index of clinical suspicion is required to make a diagnosis and laparoscopic approaches to remove the trichobezoar from the stomach and small bowel are safe and feasible.
Author contributions
All authors were involved in the patient’s care and made contributions to the writing of the final manuscript.
Conflict of interest statement
None declared.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.



