-
PDF
- Split View
-
Views
-
Cite
Cite
Krishna Patel, Jordyn Perdue, Jaya Varre, Vinnie Serapiglia, Anthony Rizzo, Thomas Sonnanstine, Operative technique for a successful laparoscopic en-bloc resection of gastrogastric fistula following roux-en-Y gastric bypass, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad569, https://doi.org/10.1093/jscr/rjad569
Close - Share Icon Share
Abstract
Gastrogastric fistulas are rare complications following Roux-en-Y gastric bypass surgery and are characterized by a fistulous connection between the gastric pouch and the remnant stomach. The presentation is often variable and a high-index of suspicion must be maintained for accurate and timely diagnosis. In this case report, we provide a detailed review of the technical steps taken to successfully resect a gastrogastric fistula en-bloc laparoscopically with an unremarkable post-operative course.
Introduction
The Roux-en-Y gastric bypass (RNYGB) has emerged as one of the most efficacious and popular bariatric procedures to combat the global obesity epidemic [1]. As a restrictive and malabsorptive surgery, it offers a nearly 60–70% reduction of excess weight by 12 months post-operatively [2]. Many studies have also corroborated significant decreases in obesity-related comorbidities such as diabetes, hypertension, dyslipidemia, obstructive sleep apnea, urinary incontinence, cancer, and all-cause mortality [3, 4].
A gastrogastric fistula (GGF) is an uncommon post-operative complication following RNYGB and represents an abnormal connection between the surgically created gastric pouch and the excluded remnant stomach [5]. Historically, nearly 50% of non-divided gastric bypasses were complicated by GGF [6]. Although the true current incidence of GGF is difficult to ascertain, recent studies have reported a dramatic reduction in GGF incidence to ˂2% in patients with a divided RNYGB [7].
The presentation of GGFs is highly variable and a high index of suspicion must be maintained for accurate and timely diagnosis. Symptomatology can include nausea/vomiting, epigastric pain, gastrointestinal bleeding, and weight regain though some patients may remain completely asymptomatic [8, 9]. The management of a GGF depends on the symptoms, size, and location and can involve a combination of medical, endoscopic, or surgical interventions [10, 11]. In this manuscript, we demonstrate the operative technique undertaken to surgically resect a GGF in a patient with a history of a RNYGB.
Case report
The patient is a 55-year-old female with a pre-operative BMI of 47.2 who underwent a laparoscopic RNYGB (150 cm retro-colic & retro-gastric roux limb) in 2014. She presented to the emergency department with a few days of nausea and hematemesis with melena in the setting of chronic epigastric pain, reflux, and weight re-gain of 10.4 kg over the last several months. Lab work including hemoglobin was unremarkable at 13.7 g/dL. The patient denied use of nicotine or tobacco products, steroids, or non-steroidal anti-inflammatory drugs (NSAIDs).
She underwent a CT of her abdomen and pelvis that showed concern for a possible gastrogastric fistula (Fig. 1) that was confirmed via an upper GI series demonstrating the passage of oral contrast into the remnant stomach (Fig. 2). Subsequent esophagogastroduodenoscopy (EGD) also revealed an ulcer at the site of the GGF (Fig. 3). The patient was discharged home on Omeprazole twice daily. She was seen in the outpatient setting with bariatric surgery and scheduled in 3 months for laparoscopic take-down of her gastrogastric fistula.
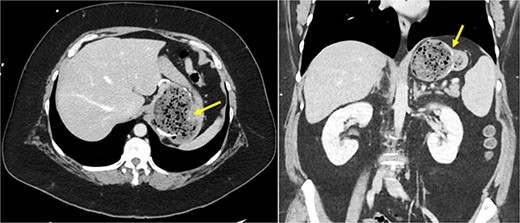
Cross-sectional CT imaging demonstrating concern for gastrogastric fistula.
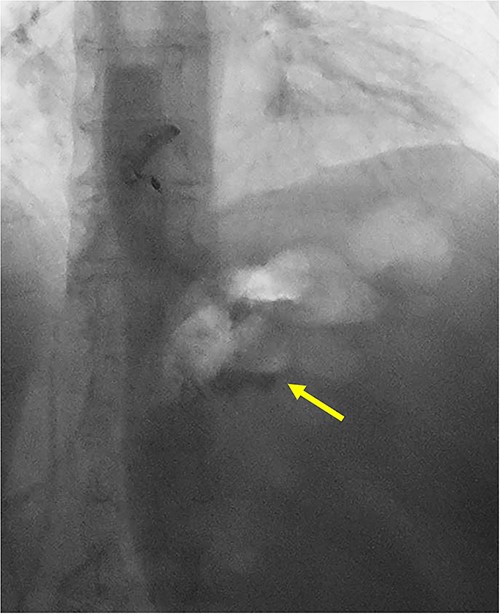
UGI series demonstrating passage of oral contrast from gastric pouch to remnant stomach.
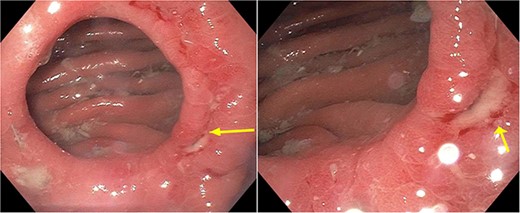
Pre-operative EGD demonstrating wide-mouthed gastrogastric fistula with an associated ulcer.
Her abdomen was safely entered periumbilically utilizing the direct OptiView technique. Two additional ports were placed under laparoscopic visualization in each hemi-abdomen and an additional subxiphoid incision was created for placement of a Nathanson liver retractor. Significant adhesions were encountered between the remnant stomach greater curvature that were carefully dissected from their attachments at the level of the mid-body to the Angle of His.
This was completed via a combination of laparoscopic scissors and Harmonic Scalpel and consequently revealed a healthy retro-gastric roux limb and gastrojejunal (GJ) anastomosis.
An intra-operative EGD was performed to assist with localizing the GGF and demonstrated a wide-mouthed fistula ~2 cm proximal to a widely patent GJ without an associated marginal ulcer. Purple cartridges on the Signia staple gun were then used to divide the remnant stomach at the level of the mid-body as well as the lateral aspect of the gastric pouch. Extreme care was taken to ensure the GJ and roux limb were preserved and not injured during this step. The en-bloc GGF specimen was removed and inspected on the back table demonstrating the fistulous connection between the remnant stomach and gastric pouch, ensuring a complete resection of the fistula (Figs 4 and 5). The total operative time was 1 h and 21 min.
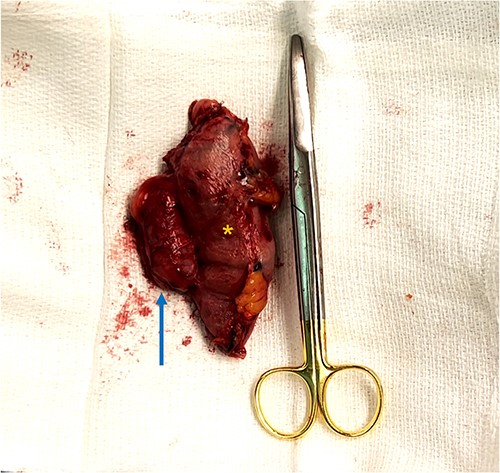
En-bloc resection of gastrogastric fistula with excised portions of gastric pouch (arrow) and gastric remnant (asterisks).
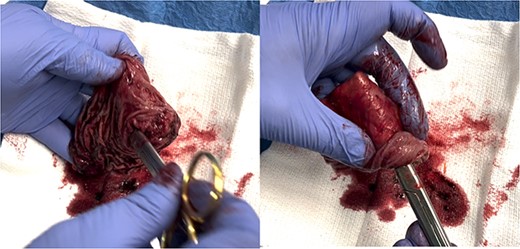
Scissors placed through gastrogastric fistula demonstrating complete resection of fistula.
The patient tolerated the procedure well and was successfully extubated post-operatively. She was given clear liquids post-operative day 0 with advancement to full liquids on post-operative day 1. She was discharged home on post-operative day 2 with appropriate pain control and Omeprazole BID and Misoprostol QID.
Discussion
Gastrogastric fistulas are a rare but known complication of RNYGB but their true incidence is underestimated in literature [10, 12]. Patients may be asymptomatic or can present with non-specific symptoms (e.g. emesis, gastrointestinal bleeding, epigastric pain, or weight re-gain) and a high index of suspicion should be maintained for appropriate diagnosis [8, 9].
The medical management of GGFs involves the eradication of Helicobacter pylori if present, avoidance of NSAIDs and smoking, and medications to reduce the effects of gastric acid (e.g. sucralfate, and high-dose proton pump inhibitor) with successful resolution in 20% of small caliber GGFs in one study [10]. Various endoscopic procedures have also been described and include fibrin sealant, endoclips, covered stents, and endoscopic suturing but are frequently associated with low success rates [12–15].
Surgical resection remains the gold-standard treatment for large and persistent GGFs that are often refractory to medical and endoscopic treatment [12]. The surgical dissection detailed above showcases the technical nuances and steps needed to treat this complication successfully and safely and can serve as an invaluable resource to surgeons, residents, and other medical professionals. Through the dissemination of our experience, we hope to promote collaborative learning, enhance patient care, improve treatment outcomes, and ultimately contribute to the advancement of bariatric surgery.
Conflict of interest statement
None declared.
Funding
None declared.



