-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Alwatari, Ahmed Khalaf, Mohammed Alghannami, Maryam Alwattary, Agenesis of flexor pollicis longus without thenar hypoplasia: a case report and literature review, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad564, https://doi.org/10.1093/jscr/rjad564
Close - Share Icon Share
Abstract
We present a case of congenital of flexor pollicis longus agenesis without thenar hypoplasia in a 12-year-old girl with no history of trauma. Two-staged corrective surgery was planned. In the first stage, the flexor pulley was reconstructed using silicone followed by the second stage 3 months later when flexor pollicis longus reconstruction was performed using tendon transfer of the flexor digitorum superficialis. The patient completed post-operative physiotherapy and the result of the surgical treatment in both functional and cosmetic aspects was, in the authors’ opinion, excellent.
Introduction
The flexor pollicis longus (FPL) muscle acts to flex the thumb at the interphalangeal joint (IPJ) and is innervated by the anterior interosseous nerve, which is a branch from the median nerve [1]. FPL agenesis is very rarely reported in the literature and its association with normal thenar muscles is even rarer [2].
Most reported cases in the literature are in children [3]. Rarely, patients present later in adulthood life as some are reluctant to undergo corrective surgical procedure with the required post-operative physiotherapy and rehabilitation, and some patients are already accustomed to the deformity [4]. Despite its rarity, FPL anomaly has clinical significance on the patient’s hand functionality and it’s an important differential diagnosis to consider in a patient who is unable to flex the IPJ of the thumb. The deficiency of FPL is usually unilateral, but can rarely be bilateral [5–8].
Case report
A 12-year-old, right-hand dominant, female presented with a long-standing inability to flex her left thumb at the IPJ. She did not recall a history of recent or remote prior trauma. On examination we found an absence of active thumb flexion; however, passive flexion was present at the IPJ (Fig. 1).
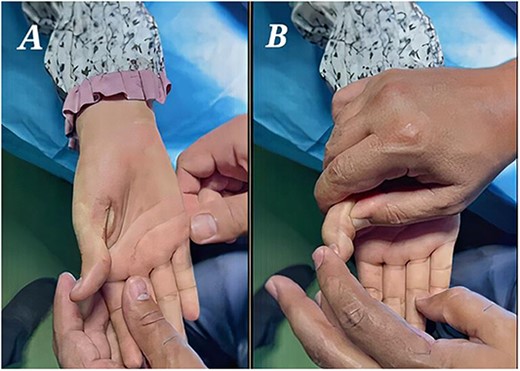
(A) Preoperative picture demonstrating an absence of flexion creases with normal thenar muscles. (B) Preoperative normal passive flexion.
Movements of all other joints of the hand were normal. The hand radiograph was normal. The inability to flex the IPJ of the thumb and the absent flexor crease of the thumb led us to clinically diagnose FPL agenesis. Two-staged surgery was planned; in the first stage, the flexor pulley was reconstructed, Reconstruction was done by silastic rod placement with reconstruction of the pulley system. Three months later, FPL reconstruction was done using tendon transfer of the flexor digitorum superficialis (FDS) tendon of the ring finger and attached to the silicon rod, which was later removed (Fig. 2).

Intraoperative pictures of the second stage of surgery that included tendon transfer and silicon removal.
Post-operative physiotherapy was performed to improve the range of motion (ROM) of the IP joint. Six months later, the thumb active flexion was possible proximally 55°–70° at the IPJ with normal thumb opposition (Fig. 3).

(A) Excellent post-operative flexion of the IPJ proximally 55°–70°. (B) Normal thumb opposition.
Full active extension has been maintained. The patient was able to perform numerous precision activities that she was unable to do previously.
Discussion
Congenital inability to flex the IPJ of the thumb can result from congenital absence of the FPL, anomalous insertion of FPL, congenital tenovaginitis of the flexor tendon sheath, partial anterior interosseous nerve paralysis, traumatic rupture of FPL, and anomalous band connecting tendons. Among these, the congenital absence of the FPL without hypoplasia of the thenar muscles is the rarest variation [5, 9]. Urchida et al. [2] proposed the following classification for congenital FPL anomalies:
FPL without thenar muscle hypoplasia: (i) Absence, (ii) Anomalous insertion, (iii) Abnormal connection.
FPL with hypoplasia of the thenar muscles: (i) Absence, (ii) Malposition.
Our case involved absent muscle without thenar hypoplasia that is very rare. Eleven cases have been reported in the literature with similar presentations. The majority of the patients were children with unilateral disease (Table 1). Ultrasound scan has been recommended as the initial diagnostic modality [9] although most patients were diagnosed clinically and some required electromyography testing. Surgical reconstruction followed by rehabilitation has been the treatment of choice and achieved average active flexion of ~40°; Tow staged operative surgery overall showed better results.
| Author/year . | Age/sex . | Diagnosis . | Surgical Treatment . | Active flexion results . |
|---|---|---|---|---|
| Miura, T./1977 [10] | 1y/F | Clinical | One stage tendon transfer | 20° flexion |
| Arminio, J. A./1979 [11] | 6y/F | Clinical | Two-staged tendon transfer | 25° flexion |
| Koster, G./1984 [12] | 13y/F | Clinical/EMG | Two-staged tendon transfer | 35° flexion |
| Urchida et al./1985 [2] | 7y/F | Clinical/EMG | One stage tendon transfer | 35° flexion |
| DeHaan, M. R. et al./1987 [13] | 5y/M | Clinical | Two-staged tendon transfer | 55° flexion |
| Thomas C, Mathivanan/1999 [3] | 11y/F | Clinical | One stage tendon transfer | 25° flexion |
| Alicioglu, B./2007 [9] | 10y/M | US/MRI | Not reported | Not reported |
| Demirseren, M. E et al./2007 [5] | 14y/F | Radiograph/MRI | Not reported | Not reported |
| Suresh, S. S. et al./2009 [4] | 25y/M | Clinical/US | Not reported | Not reported |
| Kumar R. et al./2020 [7] | 30y/Fa | MRI | Not reported | Not reported |
| Meeuwis, I. H. M. et al./2022 [8] | 23y/Fa | MRI | Not reported | Not reported |
| Present case | 12y/F | Clinical | Two-staged tendon transfer | 55°–70° flexion |
| Author/year . | Age/sex . | Diagnosis . | Surgical Treatment . | Active flexion results . |
|---|---|---|---|---|
| Miura, T./1977 [10] | 1y/F | Clinical | One stage tendon transfer | 20° flexion |
| Arminio, J. A./1979 [11] | 6y/F | Clinical | Two-staged tendon transfer | 25° flexion |
| Koster, G./1984 [12] | 13y/F | Clinical/EMG | Two-staged tendon transfer | 35° flexion |
| Urchida et al./1985 [2] | 7y/F | Clinical/EMG | One stage tendon transfer | 35° flexion |
| DeHaan, M. R. et al./1987 [13] | 5y/M | Clinical | Two-staged tendon transfer | 55° flexion |
| Thomas C, Mathivanan/1999 [3] | 11y/F | Clinical | One stage tendon transfer | 25° flexion |
| Alicioglu, B./2007 [9] | 10y/M | US/MRI | Not reported | Not reported |
| Demirseren, M. E et al./2007 [5] | 14y/F | Radiograph/MRI | Not reported | Not reported |
| Suresh, S. S. et al./2009 [4] | 25y/M | Clinical/US | Not reported | Not reported |
| Kumar R. et al./2020 [7] | 30y/Fa | MRI | Not reported | Not reported |
| Meeuwis, I. H. M. et al./2022 [8] | 23y/Fa | MRI | Not reported | Not reported |
| Present case | 12y/F | Clinical | Two-staged tendon transfer | 55°–70° flexion |
aThese two cases were bilateral in which surgical treatment is contraindicated.
| Author/year . | Age/sex . | Diagnosis . | Surgical Treatment . | Active flexion results . |
|---|---|---|---|---|
| Miura, T./1977 [10] | 1y/F | Clinical | One stage tendon transfer | 20° flexion |
| Arminio, J. A./1979 [11] | 6y/F | Clinical | Two-staged tendon transfer | 25° flexion |
| Koster, G./1984 [12] | 13y/F | Clinical/EMG | Two-staged tendon transfer | 35° flexion |
| Urchida et al./1985 [2] | 7y/F | Clinical/EMG | One stage tendon transfer | 35° flexion |
| DeHaan, M. R. et al./1987 [13] | 5y/M | Clinical | Two-staged tendon transfer | 55° flexion |
| Thomas C, Mathivanan/1999 [3] | 11y/F | Clinical | One stage tendon transfer | 25° flexion |
| Alicioglu, B./2007 [9] | 10y/M | US/MRI | Not reported | Not reported |
| Demirseren, M. E et al./2007 [5] | 14y/F | Radiograph/MRI | Not reported | Not reported |
| Suresh, S. S. et al./2009 [4] | 25y/M | Clinical/US | Not reported | Not reported |
| Kumar R. et al./2020 [7] | 30y/Fa | MRI | Not reported | Not reported |
| Meeuwis, I. H. M. et al./2022 [8] | 23y/Fa | MRI | Not reported | Not reported |
| Present case | 12y/F | Clinical | Two-staged tendon transfer | 55°–70° flexion |
| Author/year . | Age/sex . | Diagnosis . | Surgical Treatment . | Active flexion results . |
|---|---|---|---|---|
| Miura, T./1977 [10] | 1y/F | Clinical | One stage tendon transfer | 20° flexion |
| Arminio, J. A./1979 [11] | 6y/F | Clinical | Two-staged tendon transfer | 25° flexion |
| Koster, G./1984 [12] | 13y/F | Clinical/EMG | Two-staged tendon transfer | 35° flexion |
| Urchida et al./1985 [2] | 7y/F | Clinical/EMG | One stage tendon transfer | 35° flexion |
| DeHaan, M. R. et al./1987 [13] | 5y/M | Clinical | Two-staged tendon transfer | 55° flexion |
| Thomas C, Mathivanan/1999 [3] | 11y/F | Clinical | One stage tendon transfer | 25° flexion |
| Alicioglu, B./2007 [9] | 10y/M | US/MRI | Not reported | Not reported |
| Demirseren, M. E et al./2007 [5] | 14y/F | Radiograph/MRI | Not reported | Not reported |
| Suresh, S. S. et al./2009 [4] | 25y/M | Clinical/US | Not reported | Not reported |
| Kumar R. et al./2020 [7] | 30y/Fa | MRI | Not reported | Not reported |
| Meeuwis, I. H. M. et al./2022 [8] | 23y/Fa | MRI | Not reported | Not reported |
| Present case | 12y/F | Clinical | Two-staged tendon transfer | 55°–70° flexion |
aThese two cases were bilateral in which surgical treatment is contraindicated.
The preferred surgical reconstruction technique has been one- or two-staged tendon transfer using the FDS tendon of the ring finger. Post-reconstruction physiotherapy is vital for these patients [5, 6]. Tsuchida et al. suggested proceeding with reconstructive surgery in children when they are older than 2 years [14]. In our case, the two-stage procedure, using a silicone rubber rod and pulley reconstruction, followed by transfer of the FDS tendon of the ring finger yielded an excellent functional result.
Acknowledgments
Special thanks to Ibrahim Ahmed Ibrahim and Mohammed Jasim Alfeehan for being side to side with the surgeon in the surgery and afterword patient physiotherapy.
Author contributions
All authors contributed to the paper conception and design, collection and assembly of data, manuscript writing and final approval of manuscript.
Conflict of interest statement
None declared.
Funding
Non declared.
Data availability
The author confirms that all data generated during this study are included in this article and are available for open access.



