-
PDF
- Split View
-
Views
-
Cite
Cite
LongHai Jin, Krishanth Naidu, When you hear hoofbeats, think horses before zebras – a case of recurrent small bowel obstructions with a twist, Journal of Surgical Case Reports, Volume 2023, Issue 10, October 2023, rjad555, https://doi.org/10.1093/jscr/rjad555
Close - Share Icon Share
Abstract
Mechanical small bowel obstructions (SBOs) account for a considerable proportion of hospital admissions for acute abdominal pain. SBOs are most frequently caused by adhesions; and very few SBOs are associated with intraperitoneal devices. An 84-year-old man was admitted to our tertiary institution with recurrent SBOs that were initially believed to be caused by his implantable cardioverter defibrillator which had undergone intraperitoneal migration. However, this was later found to be a misguided ‘zebra’; as the cause was revealed to be a common ‘horse’ — adhesions. This article shares our key learnings from this diagnostic dilemma.
Introduction
Mechanical small bowel obstructions (SBOs) have an array of aetiologies, which can be classified into extrinsic (external compression onto the bowel), intrinsic (compression from within the bowel wall), and intraluminal (obstruction from within the bowel lumen). Adhesions are the most common aetiology; and intraperitoneal devices are very rare. This article presents an elderly man who presented to our hospital with recurrent SBOs caused by adhesions; however, the diagnosis was initially misguided by an unusual migrating intraperitoneal implantable cardioverter defibrillator (ICD).
Case report
An 84-year-old man was admitted three times to our tertiary institution within six weeks with recurrent SBOs. He presented on each occasion with acute colicky abdominal pain, vomiting and obstipation. His examination revealed abdominal distension and periumbilical tenderness without signs of peritonism. His comorbidities included ischaemic heart disease with previous triple coronary artery bypass grafts, atrial fibrillation, chronic obstructive pulmonary disease and rheumatoid arthritis. Surgically, he had a pyloroplasty as an infant; as well as an open appendicectomy and a laparoscopic cholecystectomy several decades ago. Furthermore, he had an ICD (Medtronic XT VR DVBB2D1) placed in the left preperitoneal space two years ago for recurrent ventricular fibrillation. His pectoral anatomy had precluded a standard pectoral ICD placement. Interestingly, he has had six episodes of SBOs and all of them had occurred following the ICD placement.
The abdominal computed tomography (CT) studies on all three recent admissions were consistent with SBO. The transition point was consistently seen in the right iliac fossa; with small bowel loops distended proximally with air-fluid levels and faecalised contents; and small bowel loops collapsed distally to the ileocaecal valve (Fig. 1A). There were no signs of bowel ischaemia or perforation. However, the preperitoneal ICD appeared to have migrated into the peritoneal cavity (Fig. 1B). On review of the serial abdominal CT studies over the past two years, the ICD was in a different intraperitoneal location each time (Fig. 2). The recurrent episodes of SBOs were thus believed to be related to the ICD, due to either intraperitoneal migration of the device or formation of adhesions from its placement, given the coinciding timeline.
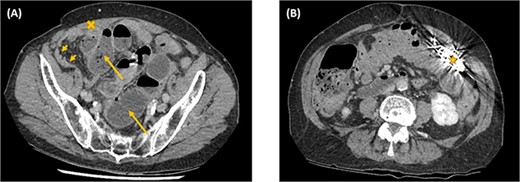
Axial computed tomography images showing small bowel obstruction with a transition point in the anterior right iliac fossa (cross). There are distended small bowel loops proximally with air-fluid levels and faecalised contents (arrows); and collapsed small bowel loops distally (arrow heads). The ICD is located intraperitoneally (star).
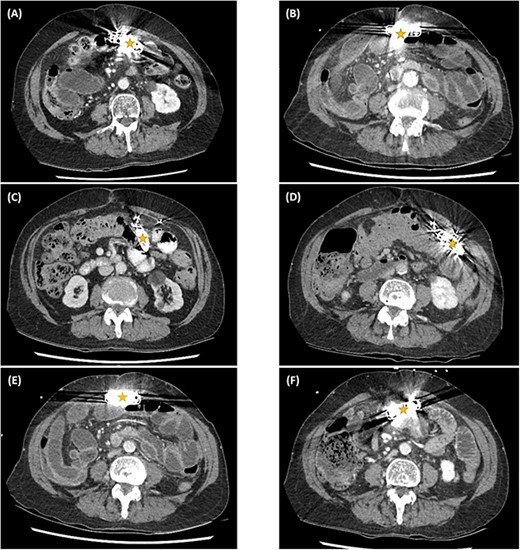
Serial computed tomography studies from the six episodes of SBOs showing the abdominal ICD device (star) in a different intraperitoneal location each time — in March (A), April (B), and November (C) of 2019; November (D) and December (E) of 2020; and January (F) of 2021.
For the first and second hospital admissions, he was managed non-operatively with nil-per-oral, nasogastric tube decompression, intravenous fluids and electrolytes. He successfully passed Gastrografin follow-through into the colon (Fig. 3A). His diet was then progressed and he was discharged home. For the third admission, he did not pass Gastrografin follow-through (Fig. 3B). His treatment was escalated for several indications, including the frequency of SBO recurrences, suspected intraperitoneal migration of the ICD, non-progression of Gastrografin follow-through and non-resolution of obstructive symptoms. He underwent a laparotomy to surgically relieve the mechanical obstruction. Intraoperatively, dense matted adhesions were found between loops of small bowel in the right iliac fossa. Although the ICD was freely floating within the peritoneal cavity, but it did not cross to the right side to have direct involvement with the mechanical transition point. Extensive adhesiolysis was performed to release the mechanical transition point of the small bowel. The ICD was then resecured in a new retrorectus pocket on the left abdominal wall. His postoperative recovery was uneventful and he was discharged home a week later.
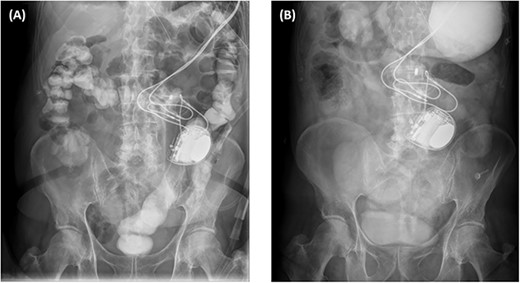
X-ray plain films of the abdomen showing passage of Gastrografin into the colon and rectum during the first admission (A); and the non-progression of Gastrografin in the stomach during the third admission (B).
SBOs account for 15% of emergency presentations for acute abdominal pain as well as 15% of gastrointestinal surgical admissions to hospital [1]. Adhesions are responsible for 65% to 74% of SBOs [1, 2]. Other mechanical causes of SBO are hernias, tumours, volvulus, intussusception and Crohn’s disease. In the absence of bowel ischaemia, perforation and peritonitis, 73 to 90% of SBOs resolve non-operatively with supportive treatment, especially with judicious use of water-soluble contrast agents like Gastrografin [3, 4]. However, SBOs can still have profound impacts on the quality of life of patients due to symptoms of pain and obstruction, as well as from discomfort associated with interventions and operations.
Placement of cardiac devices on the abdominal wall is uncommon compared to the usual pectoral placement. Migration of abdominal devices is therefore even rarer as a complication. Li et al.[5] reported on a case of intraperitoneal migration of a retrorectus cardiac pacemaker ten months following its placement in a 60-year-old woman. SBOs caused by intraperitoneal devices are also rare. A few isolated cases of SBOs have been caused by Tenckhoff peritoneal dialysis catheter, migrated hernioplasty mesh and V-Loc sutures, as well as left ventricular assist device driveline [6–10].
In medicine, there is an old saying ‘when you hear hoofbeats, think of horses before zebras’. It highlights that we should not be distracted by more exotic diagnoses (the zebras) when simple and common diagnoses (the horses) are plausible. In this case, the apparent device migration and the onset of SBOs after ICD placement clouded the diagnosis for the mechanical cause of the SBOs. In retrospect, the serial CT studies consistently showed the transition point in the right iliac fossa despite the ICD migrating around the left-to-mid peritoneal cavity. It was recognised intraoperatively that the extensive adhesions in the right iliac fossa were probably developed several decades earlier from the acute appendicitis and open appendicectomy and had remained dormant until the recent ICD placement. It is thus imperative to meticulously evaluate the previous medical and surgical histories — as they may allow an otherwise seemingly occult aetiology to be identified that would redirect the subsequent treatment.
Conflict of interest statement
None declared.
Funding
None declared.
Data availability
Data is available upon request by contacting the corresponding author.
Patient consent
Consent provided by the patient.



