-
PDF
- Split View
-
Views
-
Cite
Cite
Shing Wai Wong, Zhen Hao Ang, Philip Crowe, Improving ergonomics for the bedside assistant in robotic colorectal surgery, Journal of Surgical Case Reports, Volume 2023, Issue 1, January 2023, rjad007, https://doi.org/10.1093/jscr/rjad007
Close - Share Icon Share
Abstract
The aim of the study was to document when significant bedside assistant (BA) and robotic arm collisions occurred during robotic colorectal surgery (RCS). An observational study of 10 consecutive RCS cases, from May 2022 to September 2022, was performed. Situations when there was significant collision between BA arm and robotic arm (to cause inadvertent movement of the assistant instrument) were documented. The assistant port was randomly placed to the right or the left side of the camera port. Situations which led to detrimental BA ergonomics include dissection at the most peripheral working field, proximity of the target (mesenteric vessels), small bowel retraction, placement of the assistant port in the medial position (on the left side of the camera port), during intra-corporeal suturing and robotic stapler use. The robotic console surgeon can predictably identify and avoid situations when injury to the BA may occur.
What does this paper add to the literature?
The study is important because it is the first to document situations when the bedside assistant may be injured by the robotic arms during robotic colorectal surgery. Recommendations to improve bedside assistant access have been suggested to enhance the surgical team experience.
INTRODUCTION
Improved ergonomics for the operating surgeon may be an advantage of robotic colorectal surgery (RCS). The ergonomic benefits relating to better visualization, posture and manipulation have been studied for the console surgeon [1]. There has been little research into ergonomics for the bedside assistant (BA) in RCS. Some of the robotic ergonomic benefits may not apply to the BA because there is no three-dimensional vision and there may be restricted movement related to obstruction by the robotic arms. The console surgeon is not always aware of the position of the robot arms which can cause potential harm to the BA [2]. There are other ways that BA ergonomics may be impaired, which can impact negatively on surgery outcome. Non-verbal communication is impeded with RCS and therefore verbal communication needs to be more precise for the BA to understand directions from the surgeon [3–5].
There may be benefits for the BA related to the ability to sit down when bedside assistance is not required and less need for the shoulder to be abducted for a prolonged period when retracting from a distant port during laparoscopic colorectal surgery. Conversely, the BA may need to stand further away from the table and work with outstretched arms to avoid the projecting robot arms [6]. Ergonomic benefits of RCS for the BA include no requirement to hold the camera and availability of an instrument attached to the fourth robotic arm which can be controlled by the console surgeon for additional retraction [7]. The cognitive workload for the BA may be reduced because of these factors.
The aim of the study was to document how frequently and during which part of the surgery significant BA arm and robotic arm collisions occurred and when assistance by the BA was not possible. These situations can be potentially avoided if the console surgeon is aware of the situations when this occurs.
METHOD
Robotic surgery for colorectal disease was performed with the da Vinci Xi system in Prince of Wales Private Hospital by one surgeon. The four robotic ports were placed obliquely in a straight line as recommended by the manufacturer. The ports were spaced 6–10 cm apart. For right hemi-colectomy with intracorporeal anastomosis, Port 1 was placed in the midline 4 cm from the pubic symphysis (Fig. 1). A straight line was drawn from this port to the junction of the mid-clavicular line and left subcostal margin. Ports 2, 3 and 4 were placed on this line. For anterior resection, a line was drawn from the right femoral head and the junction of the midclavicular line and left subcostal margin (Fig. 2). Port 2 was placed where this line crosses the midline. Port 1 was placed above and ports 3 and 4 were placed below this port. The camera was inserted into robotic port 3 for the cases.
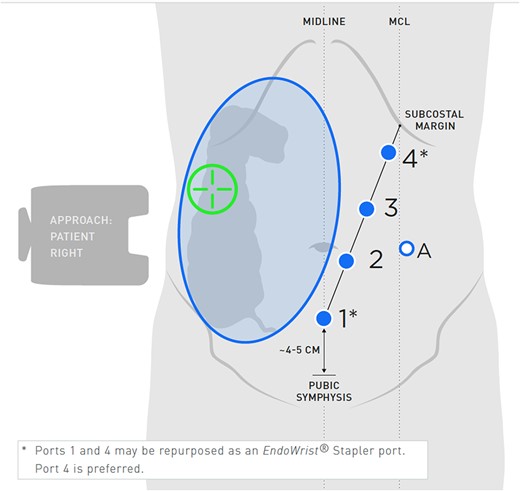
Port placement for right hemicolectomy. Adapted from: OR setup card, Intuitive Surgical Inc.
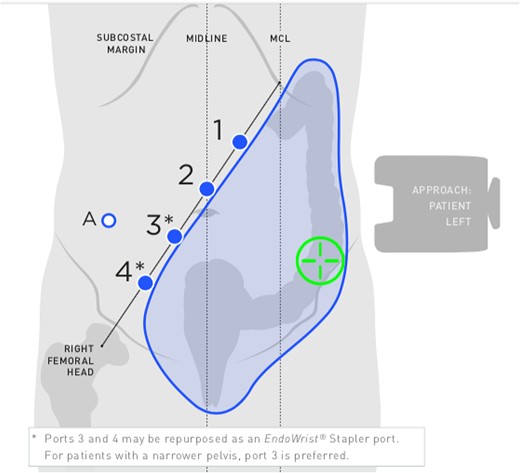
Port placement for anterior resection. Adapted from: OR setup card, Intuitive Surgical Inc.
The assistant port was placed either triangulated between robotic ports 3 and 4, or between robotic ports 2 and 3, away from the target anatomy. A short Pfannenstiel incision was performed at the start of the case and a Gelport® mini with port was inserted. This site was used to extract the colon specimen for all cases.
An observational study of 10 consecutive RCS cases, from May 2022 to September 2022, was performed. Situations when there was significant collision between BA arm and robotic arm (to cause inadvertent movement of the assistant instrument) or when BA assistance was not possible were documented. Using a sealed envelope randomization technique, the assistant port was randomly placed to the right or the left side of the camera port, to determine if position was an important ergonomic factor for the assistant. Techniques were developed to overcome situations when bedside assistance was impeded or not possible.
Ethics for this study was sought and granted by the South Eastern Sydney Local Health District HREC, reference number: 2020/ETH00281.
RESULTS
The mean age of the patients was 68 (range 48 to 84). There were three female patients and seven male patients. The mean body mass index (BMI) was 28 (range 23–34). Five patients had BMI <28. All patients had total RCS without open conversion. Five patients underwent right hemicolectomy, one extended right hemicolectomy, one Hartmann procedure, one reversal Hartmann procedure and two high anterior resection.
The total number of significant BA and robotic arm clashes was 50 and the mean number per case was 5 (range 1 to 10). BA and robotic arm clashes were more common when the assistant port was placed on the left side (compared with right side) of the camera port: 32 to 18. Clashes occurred more commonly during cases with male patients (39 time in seven males and 11 times in three females). Clashes occurred more commonly during right-sided colon resections compared with left-sided colon resections (38 in six right-sided cases and 12 in four left-sided cases). There was no significant difference in clashes in relation to BMI (25 for five patients with BMI <28 and 25 for five patients with BMI >28).
BA and robotic arm clashes occurred more commonly during dissection in the peripheral surgical field (i.e. terminal ileum and mid transverse colon for right hemicolectomy surgery, and splenic flexure and rectum for high anterior resection surgery). The total numbers for clashes during peripheral and central dissection were 28 and 10. Clashes occurred four times during dissection of the mesenteric vessels and eight times while the BA was retracting the small bowel. Clashes occurred four times with the use of the robotic 60 mm stapler and eight times while performing intra-corporeal anastomosis. The suprapubic port was used in five cases for suction in the pelvis or right retroperitoneal space when these regions were not reachable with the standard assistant port.
DISCUSSION
Placement of the assistant port in the more medial position between and behind two robotic ports increased BA and robot arm clashes. Other situations which led to detrimental BA ergonomics include dissection at the most peripheral working field, proximity of the target (mesenteric vessels), small bowel retraction, during intra-corporeal suturing and robotic stapler use. Use of a second assistant port and use of the patient clearance buttons can improve access for the BA.
Studies have reported detrimental ergonomic effects on the BA during RCS. A randomized controlled trial has shown that use of a robotic camera holder improves the posture of the assistant [8]. However, demanding neck postures was noted in BAs during 58% of robotic prostatectomy cases [9]. In a questionnaire survey, eight of the 11 BAs reported working in non-ergonomic postures for a prolonged period of time [2]. Ergonomic assessment in 13 robotic cases reported injury/bruising in 20% of BAs related to the robotic arms with accidental contact occurring on average 2.8 times (range 0–8) per case [2]. In our study of 10 RCS cases, the BA arm was compressed on average five times (range 1–10) during each case.
BA and robotic arm collisions may be reflective of the complexity of the surgical task. BA clashes may be more common during times when the console surgeon needs to concentrate more on the task and less at what might be happening at the robot–patient interface. We found dissection in the peripheral working space, right-sided colon resections, use of robotic stapler and intra-corporeal suturing to be associated with more BA arm clashes.
The robot and assistant port positions can influence BA ergonomics. Positioning of the assistant port too close to the robot ports can result in narrow working space for the BA and result in non-ergonomic twisting and bending at the wrist and elbow levels [2]. However, spacing between ports may be restricted by the size of the patient’s abdominal cavity. We have previously shown that optimal port placement for RCS can improve ergonomics for the operating surgeon [10]. For the console surgeon, port spacing distance, obliqueness of the alignment and use of different active ports can influence manipulation angles. Improving access for the console surgeon may mitigate the need for BA assistance.
There are ways to improve ergonomics for the BA: by better positioning of monitors, increasing access via more ports, having assistants at two different positions or use of more robotic arms. In our study, the additional port in the suprapubic wound was required in five cases for suction of the right retroperitoneum or the pelvis when it was not accessible from the standard assistant port. Some surgeons routinely use two assistant ports for rectal surgery to help with retraction. One unit routinely uses two BAs, one on each side [11]. Similarly, the use of an extra robotic arm in 4-arm versus 3-arm robotic surgery can result in less dependence on the BA without compromising patient outcome [12–15].
Ports placed further away from the target will reduce the range of movement of the robotic arms. This is related to the pivot point at the port/patient interface. There is potentially more risk of BA injury by the moving robotic arms in thin patients because of the fulcrum effect. Similarly, dissection of a closer target will proportionally result in wider movements of the robotic arms. This occurred on four occasions with dissection of the ileocolic vessels or the inferior mesenteric artery. We noted during our study that bedside assistance was hindered in a thin patient, especially when the robotic instruments were directly upwards because the external robotic arms were dropped down covering the assistant port.
Placement of the assistant port between the camera port and the dominant hand port (right side of the camera port) was less likely to cause clashing because of its more lateral position (of the two common assistant port locations). The BA arm clash ratio for left- versus right-sided assistant port was almost two to one. Manoeuvrability of BA instruments was better because the lateral assistant port site allows the BA hand to move more freely peripheral to the confines of the abdominal cavity.
External collisions of robot arms can be avoided using the patient clearance buttons which can drop the posterior elbows of the robot arms to allow greater motion of the arms without changing the position of the instruments inside the abdominal cavity [16]. In our study, we found that clashing occurred more commonly when dissection was performed at the more peripheral locations. Anticipation and pre-emptive use of the patient clearance button in these situations prevented clashing.
Previous experience as a BA has been shown to shorten the learning curve as the primary console surgeon because of lessons learnt on avoidance of collisions [17, 18]. With knowledge and experience gained as a BA, the console surgeon can improve the ergonomics for the BA by improving communication (giving clear instructions regarding expected large range of robot arm motion), moving the robot arms slower and being aware of the fulcrum effect (e.g. placing trocars further from the target to reduce external arm movements) [2].
Improving BA ergonomics can result in better assisting experience and performance. Improving the technical skill of the BA may enhance console surgeon performance [19]. Regular and experienced BAs may improve the experience of the surgical team by their ability to give haptic feedback information and pre-emptively use the patient clearance buttons. Use of an experienced BA has been shown to significantly shorten console surgery times [20–22]. This improved operating efficiency may be related to anticipation and active engagement [23].
There are limitations of our study. One robotic operating surgeon involved in this study impacts on the generalizability of the findings. The colorectal surgeon (SW) has performed over 150 RCS cases and has shown to be past the learning phase [24]. BA mental workloads were not evaluated in this study. Situations where the BA was not able to assist were underreported because the console surgeon would either persist without assistance or proceed to another part of the surgery.
CONCLUSION
In our study, we have identified factors which resulted in BA arm collisions during non-simulated RCS. Being aware of when BA arm clashes occur can allow the robotic surgeon to consciously avoid these situations.
DISCLOSURES
None of the authors are recipient of external funding or grants. Ethics for this study was sought and granted by the South Eastern Sydney Local Health District HREC, reference number: 2021/ETH11587.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



