-
PDF
- Split View
-
Views
-
Cite
Cite
Laura Bennett, James Gallagher, A rare case of oesophageal and gastric fundus necrosis following traumatic splenectomy, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac455, https://doi.org/10.1093/jscr/rjac455
Close - Share Icon Share
Abstract
Oesophageal and gastric fundus necrosis are rare clinical entities and have not previously been reported concurrently. This case study describes oesophageal and gastric fundus necrosis in a 71-year-old female who developed chest pain post-splenectomy for infected splenic haematoma in the context of a fall. Upper gastrointestinal endoscopy demonstrated oesophageal and gastric fundus necrosis. This was likely due to multiple factors including comorbidities, hypoperfusion, post-splenectomy state and herpes simplex virus oesophagitis. This finding is an important differential in the unwell patient with chest pain post-splenectomy and investigation with upper gastrointestinal endoscopy could be considered in the absence of another cause.
INTRODUCTION
This case study describes oesophageal and gastric fundus necrosis in a comorbid 71-year-old female who developed chest pain Day 3 post-splenectomy. Splenectomy was performed for infected splenic haematoma secondary to a fall. Oesophageal and gastric fundus necrosis are rare clinical entities and have not previously been reported concurrently [1, 2]. Specific to this case, there are limited case reports of such pathologies occurring post-splenectomy and none reporting simultaneous oesophageal and gastric fundus necrosis [3, 4].
CASE REPORT
A 71-year-old female presented to a rural hospital with generalised abdominal pain and fevers in the context of a fall 3 days prior on a background of a myeloproliferative disorder, type 2 diabetes mellitis, cerebrovascular accident (CVA), chronic kidney disease and hypertension. The patient was tachycardic, febrile and had a peritonitic abdomen on examination. A computed tomography (CT) scan demonstrated a subcapsular splenic haematoma and haemoperitoneum. Urgent laparotomy revealed a sub-phrenic abscess and infected splenic haematoma for which uncomplicated splenectomy was performed. The postoperative course was initially uncomplicated with the patient tolerating diet, opening bowels and mobilising appropriately. Day 3 postoperatively, the patient developed burning central chest pain for which cardiac investigations were unremarkable. The patient received two units of packed red blood cells for a haemoglobin of 82 and intravenous proton pump inhibitor. The patient subsequently had a 250-ml episode of haematemesis and became haemodynamically unstable. Urgent upper gastrointestinal endoscopy demonstrated oesophageal necrosis from 20 cm from the teeth to the proximal margin of the gastro-oesophageal junction, diffuse bleeding from the distal oesophagus and adherent clot at the gastric fundus. The patient was transferred to a tertiary centre where repeat endoscopy demonstrated oesophageal necrosis and a well-circumscribed area of gastric fundus necrosis (see Figs 1–3) at the site of the adherent clot. Oesophageal biopsy demonstrated herpes simplex virus (HSV) 1-associated oesophagitis. Post-endoscopy the patient developed renal failure and failed extubation in intensive care. Given the multiple comorbidities of the patient and declining functional status prior to admission the family felt further invasive measures would not be in her best wishes. The patient was transitioned to comfort care and passed away the following day.

Upper gastrointestinal endoscopy image demonstrating oesophageal necrosis.

Upper gastrointestinal endoscopy image demonstrating sparing of the gastro-oesophageal junction.
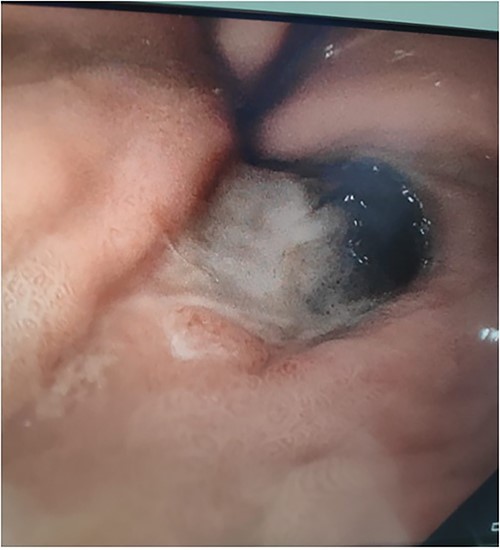
Upper gastrointestinal endoscopy image demonstrating gastric fundus necrosis.
DISCUSSION
Oesophageal necrosis is a rare diagnosis with an incidence of 0.2% annually noted in a retrospective review performed at a high volume endoscopy centre [1, 2]. It generally occurs in patients who are acutely unwell with multiple comorbidities and often in the context of ischaemic insult [2, 3, 5, 8]. Treatment is usually conservative management and prognosis is generally good [5]. Gastric fundus necrosis is an extremely rare phenomenon with unknown incidence and limited literature describing causes and best management [8]. In this case, there were multiple factors that may have led to necrosis. The patient was elderly, comorbid, post-splenectomy, had HSV-oesophagitis and at time of presentation to the emergency department was hypotensive. This state of hypoperfusion may have contributed to the occurrence of necrosis [2, 5–7]. Limited case reports on gastric necrosis post-splenectomy propose that ligation of the short gastric vessels during mobilisation of the gastro-splenic ligament combined with systemic ischaemic phenomenon can cause gastric fundus necrosis [3, 4]. Blood supply to the gastric fundus originates from multiple sources therefore ligation of the short gastric vessels does not routinely cause gastric fundus necrosis [9]. In this case, the patient may have had aberrant anatomy resulting in dependence on the short gastric arteries for supply to the gastric fundus. The other proposed mechanism for gastric fundus necrosis post-splenectomy is necrosis secondary to incorporation of tissue of the gastric wall into suture ligation of the short gastric vessels, which can be exacerbated by gastric distension in the post-operative period [10]. This mechanism is another possible explanation for this case presentation however it does not explain the concurrent oesophageal necrosis. There is sparse literature on the association of herpes oesophagitis and oesophageal necrosis however it is proposed that treatment with antivirals may improve healing in these patients therefore the presence of herpes oesophagitis may have contributed to the presentation [11]. Treatment for oesophageal and gastric fundus necrosis are generally conservative and include correction of the precipitating condition and supportive care [3, 12]. More invasive options in the event of perforation may be required including oesophagectomy or gastrectomy [3, 12].
CONCLUSION
Concurrent oesophageal and gastric fundus necrosis has not previously been described in the literature making this case extremely unique. This case was likely due to multiple factors including comorbidities, hypoperfusion, post-splenectomy state and HSV oesophagitis. This case highlights oesophageal and gastric fundus necrosis as important differentials in the unwell patient with chest pain post-splenectomy and investigation with upper gastrointestinal endoscopy could be considered in the absence of another cause.
CONFLICT OF INTEREST STATEMENT
The authors declare there are no conflicts of interest.
FUNDING
The authors declare there are no conflicts of interest.



