-
PDF
- Split View
-
Views
-
Cite
Cite
R Rathigashini, W A D P Wanniarachchi, A De Silva, R P Herath, Recurrent vaginal vault dehiscence and evisceration following total laparoscopic hysterectomy, successfully repaired with polypropylene mesh and sacrocolpopexy, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac453, https://doi.org/10.1093/jscr/rjac453
Close - Share Icon Share
Abstract
Recurrent vault dehiscence is a rare and potentially serious complication following hysterectomy. We report a rare case of recurrent vault dehiscence and evisceration following a total laparoscopic hysterectomy (TLH) which was successfully repaired with polypropylene mesh and sacro-colpopexy. A 47-year-old multiparous woman underwent TLH for adenomyosis. During the surgery, vaginal wall was incised with monopolar diathermy and sutured with synthetic absorbable barbed suture in a single layer. She presented 12 weeks later with vault dehiscence and evisceration of omentum. Laparoscopically, eviscerated omental part was removed and the vaginal cuff was repaired vaginally with absorbable synthetic suture. She came with a recurrence in 3 months with vault dehiscence and a vault prolapse without any evisceration. She underwent laparoscopic mesh repair of the vault combined with laparoscopic Sacro-colpopexy with complete recovery. Incidence of vault dehiscence is found to be higher in TLH than abdominal or vaginal hysterectomy. Treatment options for recurrent vault dehiscence involve strengthening the vault with tissues, or with a prosthesis.
INTRODUCTION
Vaginal vault dehiscence and evisceration is a rare and potentially serious complication of hysterectomy and colpotomy. With rising popularity of laparoscopic hysterectomies more cases of vault dehiscence have been recognized. Frequent use of electro-coagulation during separation of the uterus from the vaginal cuff, differences in suturing techniques and differences in suture materials (use of barbed sutures) and the technique of vault closure are presumed to contribute to the higher incidence [1]. Further, general surgical complications like vault infections, hematoma formation and lifestyle factors such as involved in heavy labor and early resumption of sexual intercourse are also being recognized as risk factors for vault dehiscence.
We report a case of recurrent vaginal vault dehiscence with evisceration occurring within 6 months of total laparoscopic hysterectomy (TLH), which was successfully managed with a laparoscopic mesh repair and sacro-colpopexy.
CASE REPORT
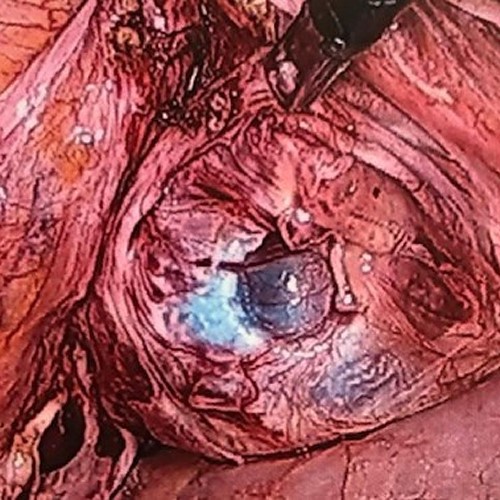
A 47-year-old woman, a mother of two, presented with irregular heavy menstrual bleeding for 1 year duration, with resulting iron deficiency anemia, not responded to medical management. Ultrasound scan revealed adenomyotic uterus without significant endometrial pathology. TLH was performed during the surgery, vaginal vault was incised with monopolar diathermy hook and sutured with absorbable barbed suture (Polydioxanone, No0) in a single layer. Intravenous ceftriaxone1g was given before induction of anesthesia and continued for 24 h. She recovered without any immediate complications. Three months later, she presented with sudden onset vaginal discharge and abdominal discomfort of 1 day duration. Vaginal examination revealed vault dehiscence and evisceration of omentum (Fig. 1). There was no vault hematoma or infection. She underwent laparoscopy, revealed total vault dehiscence with omental evisceration. Bowel looked viable with healthy peristalsis. Eviscerated part of the omentum was resected laparoscopically. The vaginal cuff was closed vaginally, by interrupted sutures after trimming the edges, using polyglactin no 1.0.Intravenous Co-amoxyclave, and metronidazole was given for 48 h.

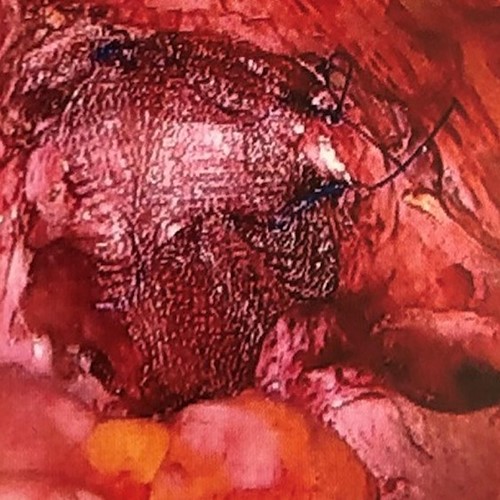
She came again 3 months later with recurrence vault prolapse and dehiscence without any evisceration. Vaginal cuff was found to be partially opened with intact thin film of tissue. Since the previous repair failed and remaining vaginal vault had a thin rim of tissues, we thought it would not provide adequate strength for a simple closure. Therefore, we decided to refresh the vaginal edges, perform two layer closure of the vaginal vault and provide additional support with synthetic nonabsorbable mesh.
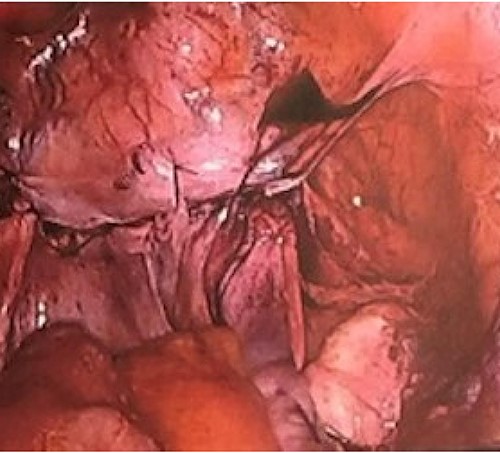
At laparoscopy, dehiscence of the vault was identified, and the peritoneal covering was opened (Fig. 2). Healed tissue at the vaginal edge was excised and both vaginal edges sutured with interrupted Polyglycolic acid No1suture, in two layers after mobilizing the bladder adequately. A nonabsorbable mesh (Polypropylene 6 × 11 cm) was placed onto the vault, extending 2 cm onto both anterior and posterior vaginal walls. Mesh was anchored to both the anterior and posterior vaginal walls with interrupted 2-0 proline (Figs 3 and 4). We used another 1.5 cm × 11cm mesh to anchor the vault to the sacral promontory. Mesh was extended via a retroperitoneal tunnel and anchored to sacral promontory with nonabsorbable helical fastener (Covidien ProTack Auto suture, 5 mm). Vaginal vault and the full extent of the mesh were completely covered with the peritoneum using Polyglycolic acid no 2.0 continuous suture. Intravenous Co-amoxyclave and metronidazole was given for 48 h. Six weeks following surgery the vaginal vault was well healed. She was followed up for 6 months and recovered completely without any long-term complications.
DISCUSSION
Vaginal vault dehiscence is a rare complication of hysterectomy. The incidence of vault dehiscence is higher after laparoscopic hysterectomy (1.14%) than after abdominal hysterectomy (0.10%, P < 0.0001, OR11.5) and vaginal hysterectomy (0.14%, P < 0.001,OR 8.3) as found in recent studies [2]. Recurrent vault dehiscence within 12 months of primary surgery is an extremely rare event and has been reported only in few case reports, where surgery was followed by radiotherapy for malignant diseases [3]. Further, resumption of sexual intercourse (8–48%) and vulsalva maneuvers (16–30%) are being recognized as important causes for vault dehiscence [4]. However, in 70% of the cases vaginal cuff dehiscence has been spontaneous without any identifiable cause [5].Our patient had resumed heavy regular activities which could have contributed to the recurrent prolapse.
In our patient during the first presentation following surgery, only the omentum was noted to be protruding out of opened vaginal vault. In case where a loop of bowel is prolapsed through the vaginal vault it must be considered as an emergency and should be attended immediately. To protect the bowel, it can be wrapped in normal saline dressings and the patient should be placed in Trendelenburg position. If the bowel is viable it is possible to reduce the bowel loop and to close the vaginal vault [3]. Bowel is deemed viable if it appears pink with contraction and good texture. We thought replacing the prolapsed omentum wound bring an infection to the peritoneal cavity and hence resected the eviscerated part.
Sound surgical technique plays a key part in preventing vault dehiscence [1, 6]. It was thought that the diathermy coagulation with consequent cell necrosis and tissue damage associated with the use of monopolar diathermy during colpotomy (diathermy with high voltage, used for coagulation) could hamper healing of the vaginal cuff. Moreover, use of extensive bipolar energy in achieving hemostasis, as in cases TLH, can cause greater tissue damage. Therefore, monopolar energy with low voltage is advised. Further, limitations of knotting associated with laparoscopy have been attributed to the increased incidence noted following TLH [6].
Suturing the vault in double layer with barbed suture or interrupted figure of eight suturing technique through vaginal approach being shown to reduce the risk. Though some believe that use of barbed sutures for closure of vault could be associated with higher incidence of dehiscence, recent meta-analysis has failed to demonstrate any disadvantages [7].
Patient should be advised to abstain from sexual intercourse and heavy manual activities until the vault is completely healed (6 to 8 weeks), and other factors which increase intraabdominal pressure should also be avoided [6].
Early initiation of broad-spectrum antibiotics and corrective surgery remains the main aspects of treatment. Surgical management should target to achieve proper tissue approximation, achieve adequate strength and address additional procedures needed such as bowel resection.
Frank et al. [8] reported two cases of recurrent vaginal vault prolapse which were successfully repaired laparoscopically using an omental flap (free or a pedunculated omental flap). Outcome following the surgeries has being satisfactory.
Our patient had very weak vaginal tissues following the initial repair. Therefore, we thought it was essential to support the vault with a mesh. We placed the mesh around the closed vaginal cuff, making further dehiscence virtually impossible. We combined this with sacro-colpopexy to prevent further vault prolapse. This worked well as inadequate vaginal strength was identified as one of the reasons for the recurrent dehiscence in our case.
Since mesh repairs are widely used for vaginal reconstructive surgeries, we think it should be considered as a primary treatment option for vaginal wall dehiscence (even with first dehiscence) following laparoscopic hysterectomy.
ACKNOWLEDGEMENT
I acknowledge the patient for providing details for publication.
INFORMED CONSENT
Informed consent has been obtained from patient to publish the clinical history and images. Patient identifying information has been removed from the images and the case report.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



