-
PDF
- Split View
-
Views
-
Cite
Cite
Ana Sofia Araújo, Sara Anacleto, Catarina Laranjo-Tinoco, Andreia Cardoso, Nuno Morais, João Nuno Torres, Miguel Mendes, Ricardo Leão, Emanuel Carvalho-Dias, Laparoscopic treatment of entero-neobladder fistula after radical cystectomy, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac419, https://doi.org/10.1093/jscr/rjac419
Close - Share Icon Share
Abstract
Entero-neovesical fistula is a rare complication of orthotopic ileal neobladder after radical cystectomy occurring in <2% of cases. Surgical treatment is usually required and includes open resection of the affected bowel tract and reconstitution of bowel transit. Here we present a case of a laparoscopic treatment of entero-to-neobladder fistula 8 years after laparoscopic radical cystectomy to demonstrate the feasibility and safety of minimally invasive treatment (Supplementary Video). To the best of our knowledge, this is the first report of minimally invasive treatment of entero-neobladder fistula.
INTRODUCTION
Entero-neovesical fistula is a rare complication of orthotopic ileal neobladder after radical cystectomy occurring in <2% of cases [1, 2]. The most typical presentation is faecaluria, pneumaturia or recurrent urinary tract infections [1]. Diagnosis is usually confirmed by contrast-enhanced abdomino-pelvic computed tomography (CT) [1, 3, 4]. Surgical treatment is usually required and includes open resection of the affected bowel tract and reconstitution of bowel transit [1].
Here we present a case of a laparoscopic treatment of entero-to-neobladder fistula 8 years after laparoscopic radical cystectomy. With this article, we aim to demonstrate the feasibility and safety of minimally invasive laparoscopic treatment of entero-to-neobladder fistula after laparoscopic radical cystectomy.
CASE REPORT
We present here a case of a 77-year-old male with a previous muscle-invasive urothelial carcinoma of the bladder treated in 2013 with neoadjuvant chemotherapy (gemcitabine and cisplatin) followed by a laparoscopic radical cystectomy with pelvic lymphadenectomy and construction of an open Studer’s neobladder. After surgery, histological analysis showed only residual in situ carcinoma. The patient had a normal body mass index and Eastern Cooperative Oncology Group of 0 with a fully active life. Besides arterial hypertension and dyslipidaemia under control with medication, he has no other relevant medical history.
After surgery, the patient presented an elevated post voiding volume and recurrent urinary tract infections with kidney function impairment and was proposed to self-catheterization. In 2017, the patient developed faecaluria. At this time, a cystoscopy was done and multiple neobladder stones were visible but no stenosis or fistulas were identified. CT scan with oral contrast revealed passage of contrast from an ileal loop to neobladder (Fig. 1a) and multiple neobladder stones (Fig. 1b) making the diagnosis of ileal to neobladder fistula. A first conservative treatment with low-residue diet and prolonged transurethral urine drainage was attempted but the fistula did not close, and the patient maintained faecaluria. We proposed the patient for minimally invasive laparoscopic repair of the fistula and removal of the stones. The pre-operative serum creatinine was 2.7 mg/dL with a glomerular filtration rate of 21.75 mL/min. Urine analysis revealed an Escherichia coli susceptible to amoxicillin–clavulanic and cotrimoxazole but resistant to cephalosporins. Antibiotic prophylaxis with 1.2 g of amoxicillin-clavulanic was administered to the patient. Preoperative bowel preparation was not done.
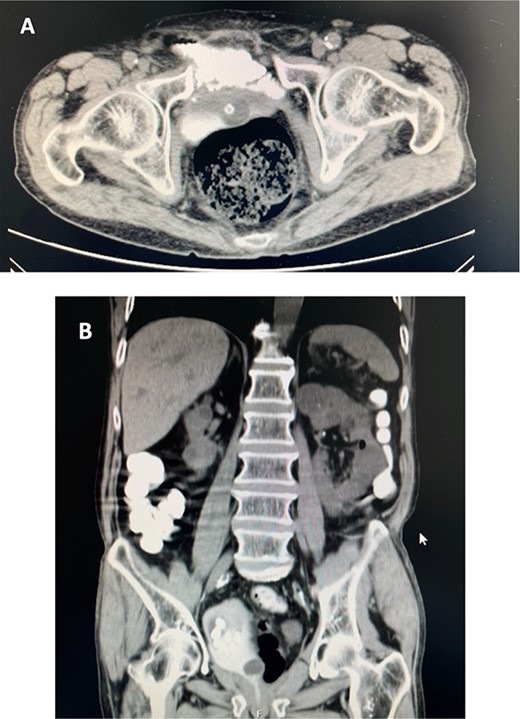
(A). CT scan with oral contrast (axial view) revealed passage of contrast from an ileal loop to neobladder. (B). CT scan with oral contrast (coronal view) showing multiple stones in neobladder.
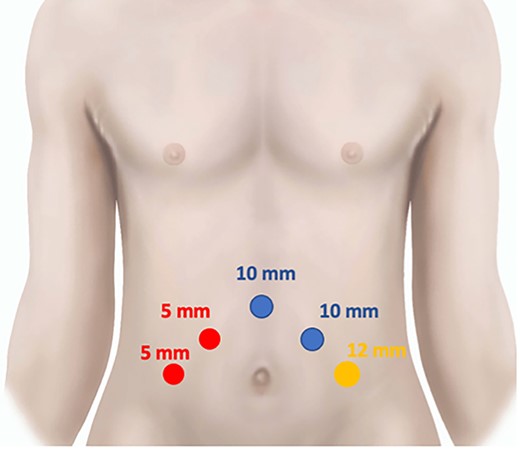
During the surgical procedure, the patient was positioned in Trendelenburg position and five trocars were introduced in abdominal cavity as shown in Fig. 2. The first step was to separate abdominal adhesions in the peritoneal cavity and suspend the sigmoid colon. After that, the ileal loop in contact with the neobladder was isolated and the neobladder was separated from iliac vessels and the ureters were safely exposed. Then, the ileal segment was cut proximally and distally with endoGYA and the segment was carefully dissected from the neobladder. After that multiple stones were removed from the opened neobladder and the neobladder was closed with a running suture. Lastly, the ileal transit was reconstructed with endoGYA stapler (Supplementary Video).
In the first 2 days, the patient remained with only intravenous fluid therapy and then, when the bowel function returned at Day 2, also started oral diet, progressing from full liquid diet to soft diet and then normal according to his tolerance. Immediate resolution of faecaluria was observed but the urinary transurethral catheter was left for 4 weeks to allow proper healing. Overall, the post-operative period was uneventful.
DISCUSSION
As there are only few cases of entero-neovesical fistula following orthotopic ileal bladder after radical cystectomy, this condition diagnostic and treatment could be very difficult and challenging.
Etiology of entero-neobladder fistulas seems to be multifactorial [2]. This patient was not diabetic, does not have signs of tumor recurrence, never had radiotherapy, neither inflammatory bowel disease nor bowel diverticular disease, so we attributed the entero-neovesical fistula to neobladder outlet dysfunction with persistent elevated post-void residual urine, stones formation and chronic distension of the neobladder.
The most typical presentation of entero-to-neobladder fistula is faecaluria, pneumaturia or recurrent urinary tract infections and the diagnosis is usually confirmed by contrast-enhanced abdomino-pelvic CT [1, 3, 4].
Conservative treatment could be the first option if the patient is stable and the fistula is small, but surgical treatment is usually required and includes resection of the affected bowel tract and reconstitution of bowel transit [1–3]. In this case, as the conservative treatment with low-residue diet and prolonged transurethral urine drainage does not work, we proceed to minimally invasive surgical treatment. Somatostatin analogues were not considered since we did not have data enough to support this clinical indication.
We demonstrate here for the first time the feasibility of minimally invasive repair for entero-neobladder fistula after radical cystectomy. Both surgeries were performed at the same center by two different surgeons with the same level of expertise in laparoscopic surgery. In fact, with the development of minimally invasive (laparoscopic or robotic) cystectomy, the rare cases of entero-neobladder fistula could also be surgically treated with a minimally invasive approach. To the best of our knowledge, this is the first report of minimally invasive treatment of entero-neobladder fistula.
CONFLICT OF INTEREST STATEMENT
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.



