-
PDF
- Split View
-
Views
-
Cite
Cite
Poh Tan, Rushabh Shah, Tarek Hassouna, Ralph Murphy, Samantha McNally, The role of biodegradable temporizing matrix in the management of a patient with major burns and anorexia nervosa, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac410, https://doi.org/10.1093/jscr/rjac410
Close - Share Icon Share
Abstract
Severe malnutrition secondary to anorexia nervosa results in deeper burns and significantly impacts wound healing, which represents a major challenge to burn management. The use of acellular dermal matrices, such as biodegradable temporizing matrix (BTM), is a valuable tool to overcome the surgical limitations. We describe a case of a 36-year-old female with a background of anorexia nervosa (body mass index of 12.3) presenting with a 30% total burns surface area (TBSA) burn. All of her burns were excised down to fascia due to the absence of subcutaneous fat. Her thin skin and depleted nutritional status significantly impacted reconstructive options. BTM was utilized to create a neodermis and provide adequate time to optimize the nutritional status before autologous skin resurfacing 3 weeks later, which yielded robust coverage with minimal donor site morbidity. Despite initial surgical and nutritional challenges, excellent outcomes were achieved in terms of wound healing, scar contractures and mobility.
INTRODUCTION
Anorexia nervosa is a severe eating disorder characterized by emaciation culminating in severe malnutrition and reduced metabolic reserve [1]. When associated with major burns, these patients are at higher risk of death due to lack of adequate physiological reserve, increased risk of sepsis and severe metabolic derangement [2, 3]. Such patients are also at risk of significantly delayed wound healing after burn injuries [4] and often have significantly reduced skin thickness, skin collagen and bone density, with minimal subcutaneous fat layers [5, 6]. This can complicate the surgical management in this cohort of patients, as the need for thin skin grafts increases the risk of subsequent wound breakdown and secondary scar contractures, while the use of standard thickness in harvesting increases the risk of donor site complications.
We utilized a fully synthetic dermal template, NovoSorb™ biodegradable temporizing matrix (BTM), to provide adequate time to optimize the nutritional requirements of the patient prior to resurfacing the neodermis with split thickness skin grafts. BTM optimized the surgical management in our patient by temporizing the wounds and reducing the risk of problematic scars and secondary contractures.
CASE REPORT
A 36-year-old woman, with a history of severe anorexia nervosa, presented to our regional burns centre with 30% flame burns over the right side of her body, including back (see Fig. 1A), right arm, neck, torso and hip (see Fig. 1B). The patient was transferred to theatre for initial debridement after undergoing immediate resuscitation. Intraoperatively, 26% of burns were of full thickness and 4% were deep dermal, with circumferential full thickness burns around the right arm. She underwent immediate escharotomy of right arm and excision of all deep burns with meshed allograft cover within the first 24 hours. Initial excision was down to fascia due to near absence of subcutaneous fat, while care was taken to preserve the right breast tissue mound.
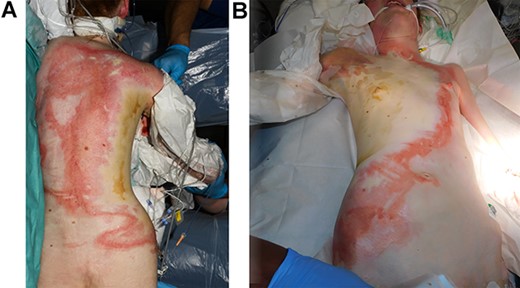
A view demonstrating the extent of the burn upon initial presentation to hospital: (A) back; (B) neck, torso and hip.
Given the depleted nutritional status (the patient had an admission weight of 36.5 Kg and body mass index (BMI) of 12.3) and increased risk of wound breakdown, a decision was made to temporize her wounds using a novel synthetic dermal matrix (BTM), ~5 days after the initial excision. The entire wound was resurfaced in one session with four sheets (20 × 40 cm each) of BTM, which was found to conform well over the breast curvature (see Fig. 2A and B). The wound surface was covered by a single vacuum-assisted closure (VAC) dressing and required six VAC machines set on 120 mm/hg. The dressings were changed every 5 days and all wound swabs were negative throughout.
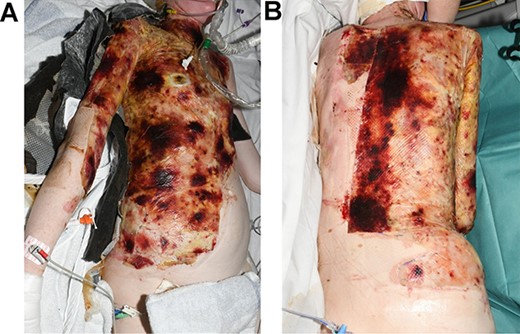
One week after the application of BTM: (A) torso, right flank and right arm; (B) back.
A personalized nutritional plan was implemented during the initial stage of her admission, and nutritional status optimized through the combined use of nasogastric (NG) and oral feeding. Overall, after 6 weeks, the patient’s weight had increased to a peak of 45.9 Kg, while her blood markers, including calcium, phosphate, copper, zinc, selenium and albumin, wholly normalized.
Twenty-eight days after the application of BTM, the patient underwent multiple procedures where the BTM was delaminated and skin grafted in stages using an electric dermatome on the smallest available setting (0.2 in 1/10 mm) to produce the least donor site morbidity. Fourteen days after the last surgical procedure, all skin grafts had fully taken (see Fig. 3A), and donor site wounds healed (see Fig. 3B and C). Eight weeks post-burn injury, the scars had started to mature with no evidence of wound breakdown or secondary scar contractures (see Fig. 4A and B). Overall, the use of BTM provided valuable time to optimize the patient’s nutritional status in addition to producing a robust, soft tissue coverage with excellent functional and aesthetic outcomes and minimal donor site morbidity compared to skin grafting alone.
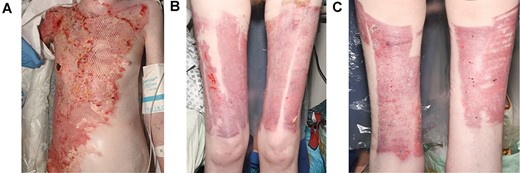
14 days after the application of split thickness skin graft: (A) good graft take to neck, chest and abdomen; (B) anterior view of healed donor sites; (C) posterior view of healed donor sites.
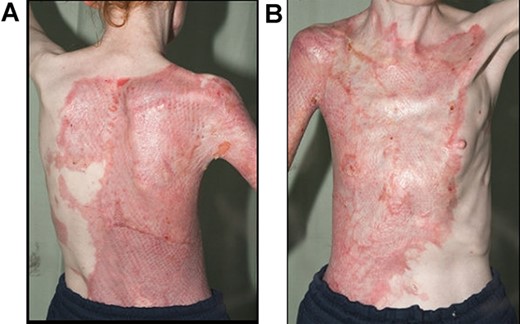
8 weeks post-application of split thickness skin graft: (A) posterior view; (B) anterior view.
DISCUSSION
Burn injuries can cause profound physiological stress on the human body, resulting in a hypermetabolic and hyperdynamic circulatory state, and if unaddressed, can lead to severe sarcopenia, immunocompromise and delayed wound healing [7–10]. The increased metabolic state from a burn injury in a patient with already low physiological reserve, seen in anorexia nervosa, complicates the management and results in poorer outcomes [9].
The reduced dermal thickness and minimal subcutaneous fat, seen in our patient, resulted in significantly deeper burns, which have limited reconstructive options [5]. Skin grafting alone can result in significant secondary scar contractures, high risk of wound breakdown and significant donor site morbidity [5]. Therefore, a decision was made to use BTM to counter this significant surgical challenge.
BTM is a 2-mm thick, synthetic dermal matrix utilized to create a graftable wound bed with the aim of recreating the inherent thickness and pliability of skin [9]. It usually involves a two-stage procedure: implantation of the bilaminar matrix allowing for host integration and creation of neo-dermis; and subsequent delamination of the superficial silicone membrane after up to 10 weeks and application of a split thickness skin graft over the vascularised matrix [10]. Furthermore, BTM has shown strong resistance to infection when associated with contamination by tracheal aspirates or faecal contamination and did not require the removal of the matrix which integrated well [11]. BTM has been demonstrated to be reliable, versatile and a safe and consistent reconstructive option in complex wounds, including acute burns, necrotising fasciitis and free flap donor site reconstruction [11].
Alternative dermal templates such as Integra® and Matriderm® are used for acute burns management to improve functional and cosmetic results [12]. However, these other acellular dermal matrices have a couple of distinct disadvantages compared to BTM. Firstly, they are made of organic material, which in case of infection or collection necessitates urgent removal, which is not the case for the entirely artificial BTM [9]. Secondly, they are remarkably more expensive than BTM [9].
To our knowledge, this is the first ever report in literature to highlight the surgical and nutritional challenges presented in the management of major burns in an anorexic patient with severely low BMI. We describe a comprehensive management strategy utilizing BTM to temporize the burn wounds and to deliver aggressive nutritional therapy prior to skin grafting. We demonstrate that BTM restores the thickness and pliability of skin after grafting thus minimizing the high risk of wound breakdown and secondary scar contractures, particularly in our patient.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICS STATEMENTS
Patient consent for publication—consent was obtained directly from the patient.
References
Author notes
Poh Tan and Rushabh Shah are joint first authors.



