-
PDF
- Split View
-
Views
-
Cite
Cite
Erica Choe, Anna Kata, Lakshmi Shree Kulumani Mahadevan, Parag Bhanot, Abdominal wall intramuscular desmoid fibromatosis: a case report, Journal of Surgical Case Reports, Volume 2022, Issue 9, September 2022, rjac401, https://doi.org/10.1093/jscr/rjac401
Close - Share Icon Share
Abstract
Desmoid tumors are rare benign myofibroblastic neoplasms that do not have metastatic potential. In this study, we report a case of a desmoid tumor in the left rectus abdominis muscle of a female patient. Computed tomography, abdominal ultrasound and magnetic resonance imaging were obtained preoperatively. We performed a complete resection with negative margins. Microscopic evaluation revealed a desmoid tumor. To definitively diagnose abdominal wall masses, imaging modalities must be used in conjunction with clinical history and histologic findings. For these masses, surgical resection is the preferred line of treatment.
INTRODUCTION
Abdominal wall masses are associated with a number of differentials and difficult to diagnose with imaging alone [1]. The clinical history and presentation are critical in the diagnostic process [2]. Common abdominal wall masses are divided into three broad categories: benign tumors (lipomas, desmoid fibromatosis, hemangiomas, neurogenic), malignant tumors (sarcomas, lymphomas, metastases) and tumor-like lesions (hernias, endometriomas, hematomas, abscesses) [3, 4]. Delineating whether the mass is fat-containing, cystic or solid is an important first step and is often achieved through ultrasound [4]. Computed tomography (CT) and magnetic resonance imaging (MRI) can narrow the differential diagnosis. Since lesions have similar features on imaging, microscopic findings are necessary for a definitive diagnosis [5].
Desmoid tumors, or aggressive fibromatosis, are benign myofibroblastic neoplasms with no metastatic potential [6]. Desmoid tumors are rare, accounting for 3% of all soft tissue tumors [6]. In one retrospective study on abdominal wall masses, desmoid tumors were the most common, accounting for 30% of the cohort [3]. These tumors are more likely to occur in females between the ages of 20 and 40 [2, 4]. Desmoid tumors share many similar clinical and radiographic features with other abdominal wall masses and have varied compositions making the diagnosis difficult with imaging and clinical history alone [1].
CASE REPORT
An otherwise healthy 43-year-old female presented to our clinic with a palpable left upper abdominal wall mass that she first noticed 1 month prior. The patient reported a surgical history of abdominoplasty, hysterectomy and appendectomy. There was no history of surgical site occurrence or recent trauma.
CT, ultrasound and MRI were obtained, revealing a 4.3 × 3.3 × 4.1 cm mass embedded in the left rectus muscle (Figs 1–3). Based on the MRI showing hyperintensity on T2 sequence and hypointensity on T1, we predicted the mass was a benign intramuscular myxoma. Informed consent was obtained and risks of the proposed surgical plan were explained. We proceeded with surgery to obtain a pathological diagnosis and curative resection. Under general anesthesia, the mass was resected with relatively free margins and only a small amount of underlying musculature was taken (Fig. 4). Knowledge of the abdominal wall anatomy was critical to avoid entry into the peritoneal cavity and potential compromise of its integrity. The soft tissue defect was reinforced using STRATTICE™ acellular dermal matrix mesh. Microscopic examination and immunohistochemistry diagnosed the mass as a desmoid tumor with negative margins and no evidence of malignancy (Figs 5 and 6). The patient was discharged and progressed well postoperatively.
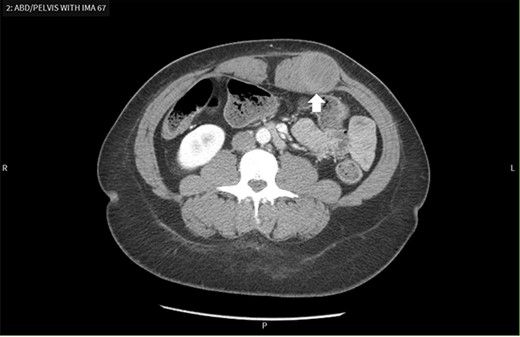
Contrast-enhanced CT scan demonstrates a mass within the left rectus sheath.
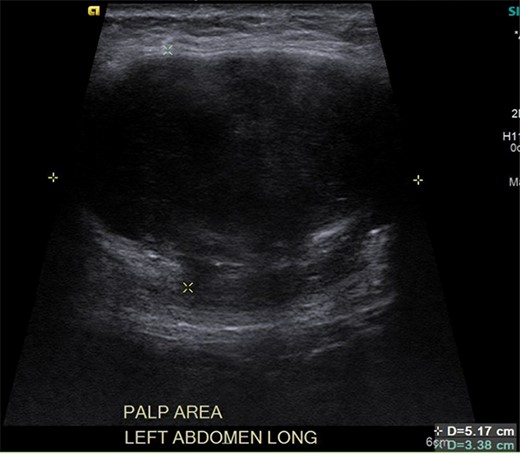
Ultrasound reveals an enlarged solid mass with internal vascularity.
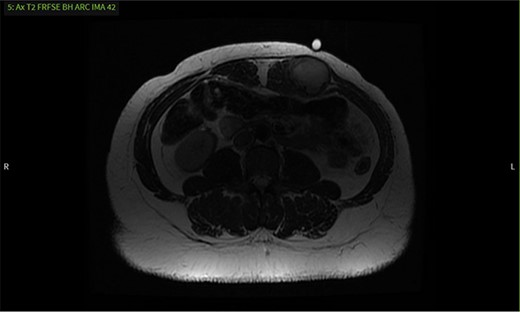
MRI shows a mass with well-defined margins and high signal intensity on T2 sequence.
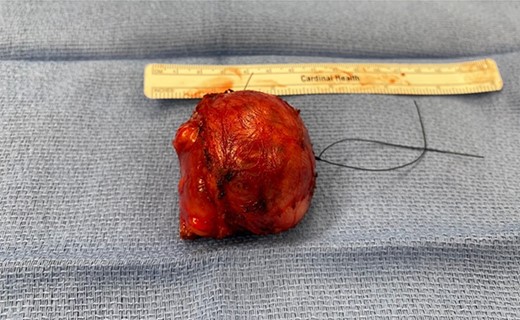
Gross specimen macroscopically shows a well-defined mass measuring 5.4 × 4.7 × 4.8 cm.
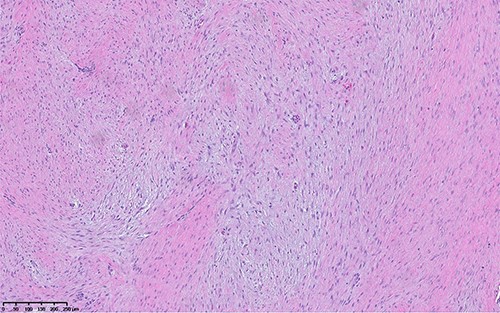
Hematoxylin and eosin image shows hypocellular lesion with long sweeping fascicles of bland spindle cells in background of collagenous and myxoid stroma.

Immunohistochemistry performed for B-catenin shows strong nuclear staining, indicating molecular alteration in CTNNB1 gene. Without the mutation, we see cytoplasmic staining.
DISCUSSION
Abdominal wall masses are difficult to diagnose based on imaging alone, as many have similar features on CT and MRI [1]. Thus, microscopic findings and immunohistochemistry are oftentimes required to confirm the diagnosis. Abdominal wall desmoid tumors are thought to arise from the aponeurosis of the anterior abdominal wall muscles embedded within either the rectus abdominis muscle, internal oblique muscle, or the fascia [4]. While they can be associated with trauma, pregnancy and familial adenomatous polyposis, more than 90% arise sporadically [2, 7].
Oftentimes, ultrasound is preferred as the first imaging modality [1]. If there is significant concern for malignancy or distant metastasis, a CT should be first [1]. In our patient, contrast enhanced CT was the first imaging modality obtained and revealed a 4.3 × 3.3 × 4.1 cm round mass low in attenuation within the left rectus sheath (Fig. 1). The mass appeared to be an intramuscular lesion with no intraperitoneal extension. A chronic seroma secondary to prior abdominal surgery or a desmoid tumor was discussed as possible differentials.
It was difficult to delineate whether the mass was primarily cystic or solid based on the initial CT, so an ultrasound was ordered. The ultrasound revealed the mass had enlarged, now measuring 5.7 × 3.6 × 4.7 cm. Internal vascularity was present, making the diagnosis of a solid mass more likely than a seroma (Fig. 2). An MRI redemonstrated the mass embedded in the left rectus muscle (Fig. 3). It had well-defined margins with high signal intensity on T2 sequence and low signal intensity on T1. On post-contrast sequences, the mass had homogeneous enhancements and a thick enhancing wall, most compatible with an intramuscular myxoma. However, without tissue biopsy, other solid tumors could not be dismissed, such as desmoid.
This is consistent with the current literature on the use of MRI as an imaging modality for desmoid tumors [1, 3]. Their presentation on MRI varies, as these tumors are thought to have early, intermediate and later stages that differ in composition [1]. In the early stage, the composition is more myxoid, with low intensity on T1 sequence and high intensity on T2, consistent with our MRI findings. At the intermediate stage, fibrous elements begin to replace the myxoid elements leading to a mixed intensity T2. Finally, in the later stage, the myxoid background is completely replaced with fibrous elements leading to low intensity on both T1 and T2. Our patient likely presented in an earlier stage and therefore had features most similar to that of a benign myxoma as opposed to a later stage desmoid tumor.
The histologic examination of the resected specimen revealed benign fibroblastic spindle cell tumors focally infiltrating into muscular tissue (Fig. 5). Immunohistochemistry revealed positivity for B-catenin and focal positivity for smooth muscle actin (Fig. 6). Ki-67 proliferation index was low (2%). The spindle cells were negative for desmin, CD34 and keratin. This was consistent with desmoid fibromatosis. The pathological assessment was critical in obtaining a definitive diagnosis.
In conclusion, while imaging modalities are important diagnostic steps in the workup of an abdominal wall mass, microscopic findings and immunohistochemistry are essential for a definitive diagnosis. While desmoid tumors can recur, complete resection with negative margins and minimal loss of surrounding musculature is the preferred treatment. Up to 20–35% of patients will have local recurrence despite surgical resection or local radiotherapy [8]. In situations where the tumor cannot be safely resected, recurs after surgical intervention or continues to enlarge with observation alone, non-surgical therapeutics such as radiation, chemotherapy, NSAIDs or antiestrogen therapies are viable next steps [1].
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



